Svetlova Olga Valentinovna
North-Western State Medical University named after I.I. Mechnikov, Russia
Title: About the possibility of another diagnosis of glaucoma and age ocular hypertension using a pneumatic analyzer ORA by criteria of rigidity and fluctuation of the scleraSvetlova Olga Valentinovna
Biography
Biography: Svetlova Olga Valentinovna
Abstract
Introduction: The issue of diagnostic division of age-related ocular hypertension (AOH) and open-angle glaucoma (OAG) today is one of the most important questions in practical ophthalmology. AOH is not actually a disease and is physiologically necessary to maintain intraocular metabolism with age. AOH is a physiological response of the eye to the gradual aging process of its structures, which leads to a continuous smooth increase in rigidity of the sclera, a decrease in its permeability and a gradual response to the growth of intraocular pressure (IOP). Similarly, arterial hypertension develops due to increased vascular rigidity. However, the classical OAG is a pathological condition, when the aging of the eye structures is ahead of the usual aging. The aging processes of the eye at OAG become abrupt: the rigidity of the sclera increases sharply by 1.5-3 times, in response IOP grows abruptly [1-3]. The practical physician is often experiencing significant difficulties with the diagnostic attempts to distinguish AOH from OAG. After all, reliable IOP means for healthy eyes with AOH and standards for eyes with OAG are not actually developed. Until recently, it was not even possible to determine which range of the true IOP norm belonged to the patient's eye at a young age: low (9-12 mmHg), average (13-16 mmHg) or high (16-22 mmHg). Therefore, the doctor is often forced to use the mythical "average pressure in the hospital", prescribing treatment without taking into account the rate of true IOP in young patients. In addition, there are no baroreceptors in the eye, so the eye does not control the pressure, but controls its volume with the help of mechanoreceptors and prostaglandin receptors of the sclera [4,5]. For a number of objective reasons in the conditions of evidence-based medicine archaic criterion of "IOP level" is no longer reliable [2,3,6]. For example, the levels of IOP in AOH in the eyes of the high-range IOP in youth or in the eyes of early stage OAG with low-range standards of IOP in youth, IOP can often be the same, although changes in the visual field and excavation of the optic disc would not be detected. And it is almost impossible to distinguish AOH and OAG from each other by means of traditional differential diagnostics. As a result, the doctor is often forced to prescribe antihypertensive drugs in both cases. However, pathogenetically poorly justified reduction of IOP in the eye by any of the known methods by 20, 30 or 40% worsens the metabolism of intraocular structures, accelerates their aging and creates prerequisites for the transition of AOH to OAG. In fact, we are using traditional methods of treatment to accelerate the transition of AOH to OAG, as well as the progression of OAG into developed stages. To reverse these negative trends new methods of differential diagnosis and treatment will need to be developed and implemented.
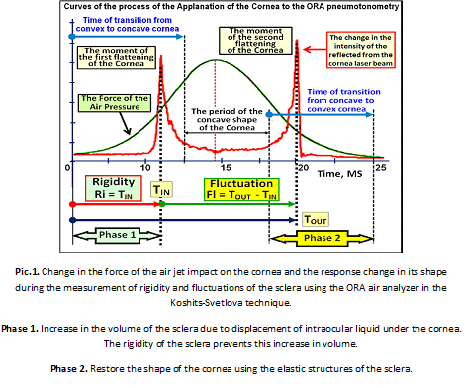
Material and Methods: The first group consisted of patients with AOH under the age of 75 years, a total of 326 healthy eyes with a high-range of IOP in youth. The second group consisted of patients aged 55-76 years with primary OAG, a total of 75 glaucomatous eyes with a low-range of IOP in youth. The level of current true IOP in both groups at the time of the examination was 23-28 mmHg For the differential diagnosis we used the modified pneumatic analyzer ORA, whose computing platform was thoroughly upgraded [1,3,7-8]. This allowed the Koshits-Svetlova method to determine in vivo the volumetric rigidity of the fibrous sheath of the eye (FSE), the true IOP according to Goldmann, the IOP level in youth, the belonging of the eye to the low-range, average, or high-range IOP rates, as well as the parameter introduced by us – scleral fluctuation (SF) [1-3,5,7-10]. In Pic. 1 the scheme shows measurement of physiological parameters of FME using our technique. SF is a new functional parameter in ophthalmology, which characterizes the ability of the sclera to restore its original shape after the pneumatic impact. SF also characterizes the functional ability of F to directly participate in the outflow of intraocular fluid, due to the retaliatory reduction of the internal volume of FSE with the help of pre-stretched elastic collagen fibers of the sclera and myofibroblasts.
Results: The increase in rigidity and decrease in scleral fluctuation with age are presented in table 1. A comparison of the values of the rigidity of FSE in healthy and glaucomous eyes within a close age group reveals significantly higher level of stiffness in glaucomous eyes than in healthy and, consequently, a lower level of fluctuations of the sclera (Pic.2).
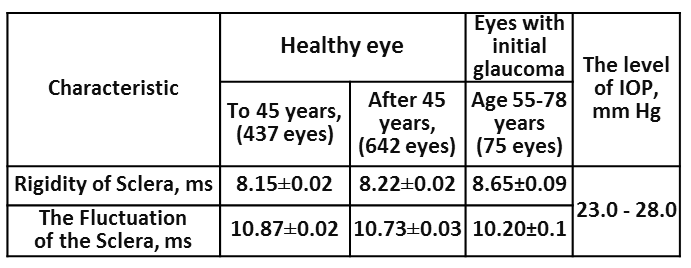
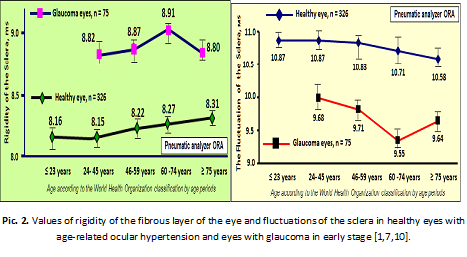
In the eye with OAG age-increased rigidity of the sclera superimposes the processes of accelerated aging of FSE, which leads to abrupt jump in rigidity and a significant reduction in the functional capacity of the sclera to fluctuate. This significantly reduces viscoelastic and functional properties of FSE in general. Moreover, the level of FSE rigidity in the glaucomatous eye already in the early stages of OAG significantly exceeds the levels of rigidity compared to healthy eyes with AOH in the elderly. But the most important thing is that the regions of finding representing the rigidity and fluctuation (Pic. 2) for AOH and OAG do not intersect anywhere. This allows reliably and objectively diagnose AOH or OAG separately from each other.
Discussion: It became clear that the development of norms/standards of rigidity and fluctuation of the sclera for healthy and glaucomatous eyes from the point of view of the physiology of the eye is much more effective than the development of standards for uncontrolled levels of IOP in the eye. After all, the fluctuation and rigidity directly characterize the current functional state of the FSE, which must be maintained independently if this is the prevention of AOH or the treatment of OAG. So restoration or maintenance of functional fluctuations of the sclera is pathogenetically justified method of treatment of the OAG or prevention of the AOH. This will ensure functional state of intraocular exchange of aqueous humor by maintaining the level of scleral fluctuation not less than 50-60% of the norm. Targeted reduction of rigidity of the sclera or the current IOP must ensure the maintenance of the scleral fluctuations at physiologically reasonable level [11,12].
References
1. Svetlova O. V., Koshits, I. N., Ryabtseva A. A. et al. The Role rigidity of the fibrous layer of the eye and fluctuations of the sclera in the early diagnosis of open-angle glaucoma.-Ophthalmol. Journal, 2010.-6:76-88. [in Russian, in English].
2. Svetlova O. V., Ryabtseva A. A., Koshits, I. N., Makarov F. N., Guseva M. G., Zaseeva M. V. About selecting effective strategies and tactics in the early diagnosis, prevention and treatment of open-angle glaucoma. Part 1. Status of the issue and assumptions.- Ophthalmol. Journal, 2014. - 2 (457): 118-133. [in Russian, in English].
3. Svetlova O. V., Ryabtseva A. A., Koshits, I. N., Makarov F. N., Guseva M. G., M. V. Zaseeva. About selecting effective strategies and tactics in the early diagnosis, prevention and treatment of open-angle glaucoma. Part 2. Theory and practice. New medical technology.- Ophthalmol. Journal, 2014. - 3 (458): 104-118. [in Russian, in English].
4. Vit V. V. The Structure of the human visual system.- Odessa, Astroprint.- 2003.- 655 P. [in Russian].
5. Svetlova O. V., Drozdova G. A., Balashevich L. I., Zaseeva M. V., Ryabtseva A. A., Makarov F. N., Koshits I. N. Morphological and physiological features of the structure of the sclera of the human eye as a key element in shaping the level of intraocular pressure in normal and glaucoma.- Morphology.- 2009.- Vol. 136.- (5): 5-10. [in Russian].
6. Gorodnjanskaja E., Svetlova O., Makarovskaia O., Pankratov R., Koshits I., Makarov F. Low confidence of the IOP criterion and clinical efficacy of OAG diagnostic by sclera rigidity and fluctuations levels and by IOP value in the youth.- 7th World Glaucoma Congress: Abstract book, 2017.- Helsinki.- P. 505.
7. Svetova O. V. Functional features of interaction of sclera, accommodation and drainage systems of the eye in glaucoma and myopic pathology. ...Diss. doctor of medical science-M., 2010.- 186 p. [in Russian].
8. Zaseeva M.V. Study of the rigidity of the sclera in healthy and glaucoma eyes.- Diss. PhD.- Military Medical Academy.- Saint-Petersburg.-2009.- 145 P. [in Russian].
9. Svetlova O. V., Koshits I. N. Physiological functions of the fibrous membrane of the eye and their Executive mechanisms. Normal and pathological physiology of the eye: monography. – Saint-Petersburg: House of North-Western State Medical University by name I. I. Mechnikov, 2014. - 64 p. [in Russian].
10. Svetlova O., Koshits I., Guseva M., Makarov F. Two key managers in the pathogenesis of OAG and innovative methods of early diagnosis.- 7th World Glaucoma Congress: Abstract book.- Helsinki, 2017.- P. 532.
11. Svetlova Olga, Koshits Ivan, Drosdova Galina. Interaction mechanisms outflow and accommodation for myopia and glaucoma. Pathophysiology: monography. -2 Edition.- St. Petersburg: Northwestern State Medical University by name I.I. Mechnikov, 2016.– 164 Ñ€. [in Russian].
12. Alla Ryabtseva, Sergey Sergushev, Roman Pankratov, Ivan Koshits, Olga Svetlova. Non-penetrating laser hypotensive sclerectomy as an alternative method of OAG treating at last stages.- 7th World Glaucoma Congress: Abstract book.- Helsinki, 2017.- P.526.

