Day 1 :
Keynote Forum
Maria A. Kovalevskaia
N.N. Burdenko State Medical University, Russia
Keynote: The effect of traditional treatment on visual function in suspected glaucoma and primary open-angle glaucoma patients
Time : 10:10-10:40

Biography:
Head of Ophthalmology Department of Voronezh State Medical Academy, Professor, General Director of "PROZRENIE" MC, AAO member Maria Kovalevskaya. She have 24 years of clinical practice like an ophthalmologist, 11 years- Head of Ophthalmologist Department of VSMA and 12 years of management experiences at Prosrenie Medical Center. She is a coauthor of the book Differential Diagnosis In Red Eye Syndrome, Alcon, author of over a dozen ophthalmology magazine articles and author of three dozen widespread interactive programmes for young ophthalmologists, including the popular CD In Red Eye Syndrome,Conjunctivitis Of Newborn, Dry Eye etc. Besides being the founder of the popular Open Source. IT medical projects 3 D CTAG Amsler Test in AMD (in collaboration with The University of California), since over a decade she is an active developer of screening in AMD, Diabetes, Glaucoma and Dry Eye development projects.
Abstract:
We evaluate the effect of traditional treatment with nasal drops Semax on visual functions in patients with suspected glaucoma and primary open-angle glaucoma, based on the color and light perception state of the results of the Farnsworth-Munsell 100 Hue and SITA-SWAP perimetry. Traditional treatment did not eliminate the disorders and did not aggravate them. Traditional treatment does not affect light sensitivity and color perception, color spectrum violations remain the same. There is a need to search for agents and methods that affect the progression of changes in the optic nerve that documented by functional tests.
- Retina and Retinal Disorders | Ophthalmology Novel Approaches | Glaucoma: Visual Field Loss
Location: Moscow, Russia
Session Introduction
Korobova Lyudmila Sergeevna
Morozov Russian Children’s Clinical Hospital, Russia
Title: Method of anesthesia for contour plasty of complicated fractures of the lower orbit wall
Biography:
Korobova Lyudmila Sergeevna is the doctor, anesthesiologist of the Department of Anesthesiology and Intensive Care; a doctor of the highest qualification category, an
aspirant.
Abstract:
Purpose: The goal is to optimize the anesthetic aid for bone-plastic operations in orbit with double access (transconjunctival or transorbital in combination with transnasal endoscopic access). The tasks are 1. To evaluate the efficacy of combined general anesthesia with sevoflurane, propofol with regional anesthesia, including: palatine access to the wing-palatal anesthesia (palatinal); infraorbital anesthesia; the van Lint block; application anesthesia; 2. To evaluate the safety this investigation.
Materials and Methods: The object of the study is children aged 4 to 17 years. Premedication is not performed. For all children in all groups, the induction of anesthesia is performed by inhaling sevoflurane through the facial mask with the preliminary filling of the respiratory circuit of the anesthesia apparatus with a gas-drug mixture with an anesthetic content of 7-8% by volume.Maintenance of anesthesia during spontaneous breathing through ETT is carried out as follows: inhalation of sevoflurane in an air-oxygen mixture with an O2 content of 40% and an anesthetic concentration of 0.7-0.9 MAK and intravenous injection of propofol at a dose of 2 mg/kg immediately after induction; regional anesthesia: anterior-temporal blockade, Wang Lint block, infraorbital anesthesia and palatine anesthesia, application anesthesia.
Results and Conclusions:
1. Stability of hemodynamic parameters
2. Refusal of narcotic drugs
3. Absence of oculocardial and oculogastral reflexes
4. Early readaptation of patients
5. Reduction of postoperative fasting time
6. Comfortable work of surgeons
Keywords: Orbit, contour plastics, regional anesthesia, infraorbital anesthesia, palatal anesthesia.
Catherine Favard
Centre ophtalmologique de l’Odeon and in Pr Brezin department, France
Title: SSOCT and SSOCT-Angiography fo the analysis of Circumscribed Choroidal Hemangiomas
Time : 11:25-11:50
Biography:
Catherine Favard, is a french retina specialist who has completed an MS degree in neuroscience at Pitie Salpetriere, working on immunolabelling of retinal cells. She has studied VEGF activity in the eye, working with Pr J. Plouet and Pr F. Malecaze. She has performed a post doc fellowship in Boston at the Scheppens Eye Institute and at Harvard University with Pr Aiello. Her main interests are diabetic retinopathy, AMD, uveitis and choroidal tumors. She is currently working at Centre ophtalmologique de l’Odeon and in Pr Brezin department at Cochin hospital where she is involved in clinical trials and publications.
Abstract:
Purpose: The longer wavelenght of swept source OCT (SSOCT), enables better penetration of retinal pigment epithelium and analysis of choroidal tumors. We present here the contribution of SSOCT and SSOCT-angiography (SSOCT-A) to the diagnosis of circumscribed choroidal hemangiomas (CH) .
Methods: 7 CH have been analysed with multimodal imaging : color fundus photography, ultrasonography (US), fluorescein (FA) and infracyanin green angiography (ICGA), and SSOCT and SSOCT-A (DRI SS-OCT Triton, Topcon).
Results : On SSOCT, all 7 CH presented the characteristic signs of CH with an acutely smooth dome-shaped tumor with thick and large spongelike choroidal vessels and partial posterior shadowing associated with subretinal fluid in 3 eyes. On SS-OCTA all cases presented an hypersignal of dilated choroidal tumoral vessels with loops, interspaced by dark areas and surrounded by an hypersignal rim. In 4 cases large abnormal tumoral vessels were observed both at the choriocapillary and choroid level, associated with choriocapillaris alterations on SSOCT and presented an ICGA late phase wash out. In 3 cases, much thinner tumoral vessels were observed on SSOCT-A below a normal choriocapillaris on SSOCT and SSOCT-A, with no late phase ICGA wash out.
Discussion and Conclusion: SSOCT and SSOCT-A enabled us to distinguish 2 types of CH : one associated with large superficial tumoral vessels could correspond to cavernous hemangiomas and one with thinner tumoral vessels below the choriocapillaris which could correspond to mixte or capillary hemangiomas. Therefore, SSOCT and SSOCT-A contribute to the diagnosis of CH and provide new insight for CH vascular pattern analysis.
Pablo Luis
Miguel Servet University Hospital, Spain
Title: The eye: A window to the brain also for Alzheimer's Disease?
Time : 11:50-12:15
Biography:
Abstract:
Purpose: To determine the usefulness of different non-invasive methods using ocular coherence tomography (OCT) for the diagnosis and follow-up of Alzheimer’s disease (AD)
Methods: Layer segmentation and linear discriminant functions were applied on a population of AD patients and age-matched controls. Patients with AD (n=150) and age-matched healthy controls (n=75) were analysed using the segmentation application prototype to automatically segment all retinal layers in a macular scan. Thicknesses of each layer were compared between patients with AD and controls and between patients with disease durations of less than or at least 3 years. Associations between retinal layer thicknesses, disease duration and AD severity were evaluated.
Results: Patients with AD had reduced thickness in the retinal nerve fibre, ganglion cell, inner plexiform and outer nuclear layers (p<0.05). The inner retinal layers were more affected in patients with long disease duration. Ganglion cell and retinal nerve fibre layer thicknesses were inversely correlated with AD duration and severity. Ganglion cell and inner plexiform layers thicknesses were predictive of axonal damage.
Conclusion: The segmentation application revealed ganglion cell and retinal layer atrophy in patients with AD compared with controls, especially in the inner layers of patients with long disease duration. Ganglion cell layer reduction was associated with increased axonal damage and may predict greater disease severity.
Martine Mauget-Faysse
Clinical Investigative Center Adolphe de Rothschild Foundation, France
Title: Optical coherence tomography angiography analysis of retinal and choroidal vascular networks during acute, relapsing and quiescent stages of toxoplasmic retinochoroiditis
Time : 12:15-12:40
Biography:
Martine Mauget-Faÿsse is a Retinal medical ophthalmologist. She did her medical studies and Certification in Ophthalmology at the University of Lyon, France, then post-doctoral training for retinal diseases at the Creteil Hospital in Paris. Since 2012, she is a medical consultant for clinical research for retinal diseases in the Adolphe de Rothschild Foundation investigation clinical Center in Paris, Principal investigator and co-investigator for biomedical protocols. Active member of numerous scientific Societies: SFO, AAO, Macula Society, Fan Club. Reviewer and author of papers on Clinical Research and Retinal diseases.
Abstract:
Purpose: To present a series of patients with clinical findings characteristic of ocular toxoplasmosis and highlight the advantages of OCT Angiography (OCT-A) in delineating the morphologic features of the retinal and choroidal vascular networks during acute, relapsing and quiescent stages of toxoplasmic necrotizing retinochoroiditis.
Patients and method: All patients diagnosed with ocular toxoplasmosis underwent a complete ophthalmic examination including a best-corrected visual acuity (BCVA) test with Snellen eye charts, intraocular pressure measurement with Goldman aplanation tonometry, anterior segment examination, and dilated fundus biomicroscopy. Standard fundus fluorescein angiography (FFA), indocyanine green angiography (ICGA), and optical coherence tomography (SD: Spectral Domain or SS: Swept Source): B, C or Angiography (Spectralis HRA Heidelberg Engineering or SS OCT Triton Topcon) were performed in all patients.
Results: Twenty three patients were enrolled. Five initial cases, 6 scarred cases and 12 cases with toxoplasmosis recurrence were analyzed. For all active retinochoroidal foci, OCT-A showed better than FFA and ICG the vessel rarefaction in the deep retinal capillary plexus (DRCP) more extensive than in the superficial retinal capillary plexus (SRCP); then on treatment, OCT-A showed the partial reappearance of these two capillary layers. On atrophic areas, the residual disorganized ischemic areas were larger in the choroidal segmented layers compared to SRCP and DRCP. EDI OCT, shows an increased choroidal thickness at the level of active foci.
Discussion: At the level of active and scarred toxoplasmosis foci, OCT-A showed better than FFA and ICG the localization and extension of retinal and choroidal capillary involvements. The partial vessel reappearance after treatment may correspond either to a vessel recanalization or to a disappearance of a masking effect induced by the active foci.
Conclusion: SD and SS OCT-A seem interesting for assessing retinal and choroidal capillary involvement in ocular toxoplasmosis. OCT-A shows that the retinal and choroidal capillary damages may be partially regressive in the initial outbreaks of toxoplasmosis treated early, which may help to better understand the pathophysiology of the toxoplasmic damage.
Waldensius Girsang
Jakarta Eye Center (JEC) Hospital, Indonesia
Title: Development of Novel Radial Relaxation Retinectomy Method on Retinal Detachment with Advanced Proliferative Vitreoretinopathy
Time : 12:40-13:05
Biography:
Waldensius Girsang is a senior consultant ophthalmologist in Retina division at Jakarta Eye Center (JEC) Hospital, the largest eye center in Indonesia. He obtained his medical doctor certification from Faculty of Medicine, University of North Sumatera and his ophthalmologist certification from Faculty of Medicine, University of Indonesia. He joined a fellowship program at JEC and Vitreoretinal Training at Zhongshan Ophthalmologic Center, Sun Yat Sen University, Guangzhou, China. He is now working due to his excellent skills as a general ophthalmologist and as a part of Cataract, LASIK, and Vitreoretina specialist team. Dr. Girsang’s clinical works focus is on diseases of the retina. His practice involves the management and surgery for retinal detachments, diabetic retinopathy and macular disorders - macular holes, epiretinal membranes, vitreomacular traction. He takes on complex retinal diseases like advanced proliferative vitreoretinopathy, trauma and retinal surgery in combination with anterior segment disease. In the field of medical retina, he manages patients with age-related macular degeneration, choroidal neovascular and polypoidal disease, diabetic retinopathy and retinal vascular diseases. His area of interest for research is in Medical Retina and Vitreoretinal Surgery, which he has presented his results of research both in national and international conferences. Currently, he is one of the scientific committee members in Indonesia Ophthalmology Association (IOA), Indonesian Medical Association [IMA] – IDI, and European Society of Retina Specialist [EURETINA].
Abstract:
Retinal detachment (RD) remains one of the most challenging cases in vitreoretinal surgery. It becomes more challenging as the condition advances, marked by abnormal cellular accumulation creating traction to the retina known as proliferative vitreoretinopathy (PVR). Treatment of RD often requires complex procedures, particularly those at advanced stage of RD with PVR. The presence of PVR may reduce the anatomical success rate of RD treatment due to double burden and difficulty level of the surgery. Surgical treatment of RD with PVR may involve multiple procedures including scleral buckling, membrane peeling, retinotomy, retinectomy and intraocular tamponande injection.
To date, vitrectomy, membrane peeling, retinotomy with additional silicon oil tamponade has been considered as the best technique for treatment of RD with advanced PVR. Retinotomy has been widely used for their management. Subsequent development of 360 degree, circumferential retinotomy was done for advanced PVR. More recently, peripheral 360 degree retinotomy, anterior flap retinectomy and radial retinotomy were combined to improve anatomical outcomes of RD with advance PVR. These techniques have been reported to have considerable anatomical success rate than previous retinotomy alone. However, recent report has suggested that only a small portion of patients achieved good visual acuity and there were substantial number of post-operative complications such as persistent hypotony, corneal damage and retinal redetachment.
Theoretically, in retinal detachment, there is tangential force caused by PVR that plays key role in creating the tractionand ultimately reduce the success rate of postoperative retinal reattachment. Therefore, any procedures performed during surgical treatment of RD with PVR should aim to reduce or eliminate this tangential force to achieve anatomical reattachment of the retina. This review aimed to show novel method of radial relaxing retinectomy to eliminate this tangential force caused by PVR, showed its anatomical success and postoperative complications of this method during 6 months follow-up.
Roberta Farci
University of Cagliari, Italy
Title: Multimodal OCT reflectivity analysis of the cystoid spaces in Cystoid Macular Edema
Time : 13:05-13:30
Biography:
Abstract:
Purpose: To compare and evaluate images of macular cysts with different degrees of reflectivity (from gray to black signal) as observed in B-scan Spectral Domain OCT (SDOCT) and En Face OCT with decorrelation signal obtained with OCT-angiography (OCTA) in eyes with cystoid macular edema (CME) secondary to diabetic retinopathy (DR) and retinal vein occlusion (RVO).
Methods: Images from 3033 patients affected by CME secondary to diabetes or RVO examined OCTA (Optovue XR Avanti, Optovue, USA) at the University Eye Clinic of Creteil, Hopital Intercommunal, France, and at the University Eye Clinic of Cagliari, “San Giovanni di Dio” Hospital, Italy, were retrospectively examined. The deep capillary plexus OCTA images and the corresponding EnFace OCT images, both acquired with the same automatic segmentation, were overlapped to compose RGB color images as red and green channels, respectively, using ImageJ software (National Institutes of Health, Bethesda, MD). Then, linear regions of interest were traced on the color images to obtain the profiles of OCTA and EnFace gray values. Number of pixels, mean gray value and standard deviation of the area traced in OCT-A and EnFace image were respectively analyzed and statistically correlated. Data were exported to Excel to create the plots.
Results: We found 94 patients with DME and 27 patients with RVO showing intraretinal macular cystoid spaces with similar homogeneous, gray-looking content, and 73 patients with DME and 113 patients with RVO showing macular cystoid spaces with homogeneous, black-looking content, as observed at SD-OCT, EnFace and OCTA scans. Interestingly, the limits of macular cystoid spaces are clearly detectable with OCTA. The analysis of red and green profiles demonstrated a clearly visible overlapping between the average OCTA and En Face signal observed around cystoid spaces, that could be attributed to a relationship between the dynamic vascularization and structural density of the tissue.
Conclusions: This is the first investigation which characterizes and correlates OCTA and enface signals on images of macular cystoid spaces in DR and RVO. The low intensity OCTA signals observed inside cystoid spaces, pose a relevant question about their nature, as to whether they are due to the presence of corpusculated material poured out from bloodocular-barrier or must be considered OCTA artifacts.
- Cornea and Corneal Diseases | Ophthalmology Surgery | Eye Research Insights
Location: Moscow, Russia
Session Introduction
José Manuel Larrosa
Miguel Servet University Hospital, Spain
Title: Could Peripapillary choroidal thickness analysis with Swept Source OCT useful for the diagnosis of glaucoma
Time : 14:30-14:55
Biography:
Abstract:
Purpose: To study peripapillary choroidal thickness (PPCT) in a wide area around the optic disc and established different zones in healthy subjects using a new swept source optical coherence tomography (SS-OCT) device. To evaluate PPCT differences between primary open-angle glaucoma (POAG) patients and age and sex marked healthy controls.
Methods: A total of 246 subjects were consecutively recruited: 111 healthy subjects and 135 glaucoma patients. The group of healthy subjects was divided in two populations: the teaching population (composed by 25 controls and used to establish choroidal zones) and the validating population (composed by 86 controls and used to compare measurements with POAG patients). An optic disc 6.0×6.0 mm three dimensions scan was obtained using Deep Range Imaging (DRI) OCT Triton. A 26×26 cube-grid centered in the optic disc is generated to automatically measure choroidal thickness. Fourchoroidal zones were established and used to compare peripapillary choroid between healthy and POAG patients.
Results: PPCT was significantly thinner in Zone 3 of POAG group, mainly located in the superior, temporal and nasal peripapillary choroid (p=0.038); and Zone 4, corresponding to the superior area, farthest from the optic disc (p=0.023). Choroid followed a similar pattern in controls and POAG; it was thicker in superior region, followed by temporal, nasal and inferior region.
Conclusions: Glaucoma patients present peripapillary choroidal thinning compared with healthy subjects, especially in farther areas from the optic disc. Peripapillary choroidal tissue shows a concentrical pattern, increasing thickness as you move away from the optic nerve. The new SS-OCT could be a useful tool to evaluate choroidal thinning and its applications in clinical practice.
Obrubov Anatoly Sergeevich
S P Botkin Moscow City Clinical Hospital, Russia
Title: The drug of choice for treatment of keratitis and corneal ulcers suspicious to the fungal etiology
Time : 14:55-15:20
Biography:
Obrubov Anatoly S MD, PhD is an Ophthalmologist of City Clinical Hospital named after S P Botkin, Moscow, Russia, and Associate Professor of the Department of Ophthalmology of Russian Medical Academy of Continuing Professional Educations, Russia.
Abstract:
Purpose: To analyze the experience of local and systemic antifungal therapy in patients with severe keratitis and corneal ulcers.
Materials and methods: For 4,5 years, 27 patients (27 eyes) were followed. The causes of the disease: wearing contact lenses – 12 patients, secondary attachment of fungal infection – 6 patients, eye trauma – 7 patients, postoperative infection – 2 eyes. 21 patients treated by 0,2% fluconazole in eye drops form and/or in subconjunctival injections (in 2 cases in combination with oral administration), 17 patients received 0,02% or 0,05% chlorhexidine gluconate solution (in 13 cases in combination with fluconazole), 5 patients – 0,3% amphotericin B in eye drops form (in 4 cases in combination with fluconazole and chlorhexidine gluconate), 2 patients – 0,1% voriconazole in eye drops form. Itraconazole was given orally in 7 cases in combination with local medications.
Results: According to the inoculation, the fungal etiology of keratitis has been confirmed in 5 cases, in others cases the etiology of the disease has not been established under laboratory condition, but in respect that the anamnesis, clinical picture and course of disease, a fungal or mixed etiology of the disease has been suggested. Surgical treatment was required for 4 patients. In 1 patient enucleation was performed (morphologically fungal etiology was confirmed). 2 patients received through keratoplasty, 1 patient was additionally treated by corneal cross-linking. In other 23 patients, persistent opacity of the cornea of varying severity was formed at the endpoint. It was not the recurrence of infection in all cases.
Conclusions: In patients with long-term keratitis and corneal ulcers with a worn-out disease pattern, the drug of choice is fluconazole. In patients with keratitis associated with the wearing of contact lenses, combined therapy of antifungal drugs in combination with chlorhexidine gluconate is appropriate. In melting of the cornea with the spread of the process inside the eye, the drugs of choice are amphotericin B and voriconazole. It is necessary to combine the methods of administration and prescribing several drugs treating a severe fungal infection of the eye.
Viktoria Serhienko
Serhienko Eye Clinic, Ukraine
Title: Changes of Physico-chemical Properties of Silicone Oil Associated with a Retinal Detachment
Time : 15:20-15:45
Biography:
Abstract:
The source material for our study was 23 samples of silicone oil, aspirated from the vitreous cavities of the eyes of patients after a tamponade about the rheumatogenic and traction retinal detachment. The average life of silicone oil in the eye was 3.5 months. In all cases, a 1300 cSt – viscosity Oxane silicone oil, Baush + Lomb, the UK, was used for tamponade. All samples were stabilized, resulting in colloidal systems consisting of a direct emulsion of two cross-saturated (aqueous and oily) liquid phases. The density of samples aspirated from the patients’ eyes was measured at a temperature of 20.00 ± 0.05°C by a pycnometric method, taking into account the adjustment for a loss of body weight in the air (0.00129 g/cm3). The viscosity measurement method using the Ostwald capillary viscometer (at a temperature of 20.00 ± 0.050°C) was used to measure the relative viscosity of samples by a three-time adjusting the viscometer for water phases against the distilled water (checking the viscosity measurement results against a 96% ethyl alcohol and acetone), and the viscometer for oil phases against a 100% dimethylpolysiloxane (checking the viscosity measuring results against glycerin). The criteria for complications were the development of proliferative vitreoretinopathy with reccurence of retinal detachment or an increase of intraocular pressure above 21 mm Hg. in the postoperative period. Depending on the density of the oil phase, patients were divided into 4 groups:
Group 1- the density of the oil phase (o.p.) – less the density of distilled water and practically corresponding to the density of silicone oil (d20 = 0.9700-0.9799 g/cm3);
Group 2- the density of the o.p. – less the water density, but greater than the density of pure silicone oil (d20 = 0.9800-0.9981 g/cm3);
Group 3- the density of the o.p. – practically equal to the density of distilled water (d20 = 0.9982-1.0049 g/cm3); and
Group 4 – density of the o.p. – above the density of distilled water (d20 = 1.0050-1.0100 g/cm3).
The study revealed that the physicochemical properties, such as the density (growing and in some cases exceeding the density of distilled water) and the viscosity (significantly decreasing), were changing in most patients (with a different magnitude) in the process of tamponade and continuous presence of silicone oil in the vitreous cavity of the eye. The density of the oil phases of aspirated samples had an exponential relation to the viscosity. The number of postoperative complications such as development of proliferative vitreoretinopathy followed by formation of a recurred retinal detachment and an increase of the intraocular pressure above 21 mm Hg. depended on the density of a silicone bubble.
Theophile Kabesha
Bukavu Eye Clinic Medical, Congo
Title: Ophthalmology practice challenges in low income countries (Eastern Congo specific case)
Biography:
Theophile Kabesha has completed his PhD at the age of 28 years from Lubumbashi University and postdoctoral studies in ophthalmology from Institute of Tropical Ophthalmology of Africa in Bamako-Mali. He also completed his studies in epidemiology and clinical research from ISPED Bordeaux-France and has been trained in medical retina at Creteil - Paris XII university ophthalmic center (France) under the ICO fellowship program sponsoring. He is the director of Bukavu eye Clinic, a provincial ophthalmologic referral center. He has published more than 10 papers in reputed journals and has been serving as the blindness prevention pioneer in eastern Congo of repute (1000 cataract surgery a year and 14000 patients performed). He actually is a professor at Bukavu official university school of medicine.
Abstract:
Ophthalmology practice in low income countries remains a very big problem up today because of inaccessibility to eye care in most of people. Blindness prevention and V2020 plan applicability in this area is up today a dream while blindness is at his highest level in most of these countries, especially in Democratic republic of the Congo. The aim of our study is to present a five years’ experience of ophthalmology practice in eastern Congo, for an advocacy for a real integration of primary eye care into the primary health care system and a support of blindness prevention program in this area. On a total 73,068 patients examination performed in our service these last 5 years, the blindness rate is 1.4 %. The blindness rate is increasing each year because of unoperated cataract (53%), uncorrected refractive errors (14.7%), glaucoma (8%), corneal pathologies, diabetic retinopathy (7.2%), traumatic pathologies (11.1%), in this area where have been made many atrocity and human right violation due to the war which destabilizes this region from 1996 up today. Many factors like the absence of qualified human resources (only 3 ophthalmologists for 8.2 millions) and specialized infrastructures (only 2 in the region), and poverty reinforces the situation. The absence of international partners and NGO involved in the eye health care in this area and no implication of the government. The national program of blindness prevention is not supported and primary eye care is not integrated in primary health care system. Prevalence of blindness is increasing in low income countries. Urgent action are required to ameliorate the situation such as training of human resources, eye care integration in primary health care system, and amelioration of eye care delivery, with government and NGO accompaniment.
Ovchar Tatyana Anisimovna
Morozov Russian Children’s Clinical Hospital, Russia
Title: Features of anesthesia for retinopathy of prematurity
Biography:
Abstract:
Proper evaluation of the general condition of a premature baby with retinopathy helps the ophthalmoanesthesiologist to choose an anesthetic for this category of patients. One group of children strictly needs an endotracheal anesthesia, in another group of patients in this age group, it is sufficient to use a laryngeal mask. What is the approach?
Purpose: To develop methods of anesthetic support for laser and surgical treatment of retinopathy of prematurity.
Materials and Methods: The number of subjects studied was 208 children, of them with moderate prematurity (31-36 weeks of gestation) -108 children, and with deep premature (24-30 weeks gestation) -100 children. 1 group (107 children) - 55 deeply premature babies with PH3+ stage-4a stage (26 patients) and PH 4b stage-5a (29 children). And 52 moderately premature patients with PH3+ stage-4a (20 patients), and with PH 4b-5 stage-32 children. 2 group (101 children) - 45 deeply premature infants with PH3+ - 4a stage (28), and PH 4b - stage 5 (17) and 56 moderately premature patients with PH3+ - 4a stage (37), and with PH 4b - stage 5 (19 patients). Children with retinopathy PH3+ stage-4a stage needed laser coagulation of the retina or they performed a shvartectomy, and prematurely with PH 4b-5 stage carried out lensswartectomy. The heavier the anamnesis of a premature patient, the greater the risk of apnea episodes in the postoperative period. This is especially true for children who have long-term ventilation, who have asphyxia in childbirth, attacks of apnea in the first month of life, in an anamnesis of BPD and IVH 2-3 st. Therefore, such children need ETA, and in postoperative supervision in the conditions of the intensive care unit. With mild and moderate morfunctional immaturity, it is possible to carry out an anesthetic aid with a laryngeal mask.
Results: In the 1st group: of the deeply premature infants, 13 children had apnea in the postoperative period, and from moderately premature infants-11. In the 2nd group, respectively, 12/9 patients.
Conclusions: ETA is administered to children with severe neonatal anamnesis, or with inadequate breathing after the installation of the laryngeal mask. The use of a laryngeal mask is an alternative to ETA at PH.
- Ophthalmology Practice | Ocular Biomechanics | Neuro-Ophthalmology
Location: Moscow, Russia
Session Introduction
Bruno Lay
ADCIS SA, Saint-Contest, France
Title: 3D Image Processing and Image Display of the Vascular Network in OCT-Angiography images
Time : 10:15-10:40
Biography:
Abstract:
Purpose: The release of new systems to capture OCT-Angiography images has opened a broad new field of image quantification directly performed on 3D volume of data. Our goal is to develop a custom and fully automatic software to display and analyze segmented 3D OCT-Angiography images, to highlight the presence of microaneurysms, ischemic areas, and to provide accurate measurements.
Methods: 3D OCT-Angiography and OCT En Face images were captured by the Spectralis system (Heidelberg Engineering, Germany). A set of 30 volumes from 15 patients was used to develop and validate the software. The volumes were exported in RAW format and opened in the software. The segmented volume is then automatically displayed in the user interface 3D viewer, along with the infra-red image and the OCT-A images. Window synchronization is available between image windows to let the user visually see the location of each image versus he other images. The user can rotate the volume in all directions, zoom in and out, alter the color of the volume and generate a movie that shows the volume in all positions. The displayed vessel network is the result of a true 3D segmentation algorithm performed on the OCT-Angiography volume. The algorithm and the result display rely on three of the 3D extensions of the Aphelion Imaging Software Suite (Image Processing, Image Display, 3D Skeletonization). The algorithm is based on morphological image processing functions. It is capable of extracting the vessel network, computing the skeleton of the vessel network, and displaying each branch of a vessel in a different user-selectable color. The software also allows to manually count microaneurysms, and to automatically compute ischemic area surface and volume vessel density.
Results: The software lets the user analyze the whole set of 30 volumes, and generate measurements on pathologies. Videos of the vessel network in the 3D space were generated and demo’ed.
Conclusion: The automatic quantification of OCT-Angiography images performed with the software was found to be very reproducible. This innovative software allows displaying OCT-Angiography images and quantifying pathologies within the same environment and user interface. The software will be adapted to other image formats captured by other systems. Future versions are currently under development to follow hardware evolution, software development regulations, as well as answering first user suggestions and comments.
Balashova Larisa Maratovna
Pirogov Russian National Research Medical University, Russia
Title: Peculiarities of cell-mediated immunity in infants with retinopathy of prematurity
Biography:
Balashova Larisa Maratovna - MD, professor, chair of library of ophthalmology of the N.I. Pirogov Russian national research medical university Ministry of healthcare of the Russian federation, NP International Sientific-Pracnical Centyre of Proliferation of the tissue of Russian federation, doctor of Morozov Russian Children's Clinical Hospital of Department of Health of Moscow. She works in the N.I. Pirogov Russian national research medical university Ministry of healthcare of the Russian federation from 1990.
Abstract:
Purpose: The goal of the present work was initiated to study the role of regulatory T cells (Tregs) СD4+СD25+Foxp3+СD127low in autoimmune disorders retinopathy (RP) in various stages of prematurely born kids.
Materials and Methods: The estimation of immunophenotype including Treg numbers in groups of mature donors (28), healthy mature and prematurely born kids with RP were compared. In total, 27 mature kids in age between 1.5 month to one year and 60 kids with RP from III+ to V active stages in age of 1.5 month to one year were studied in gestational ages from 25 to 32 weeks.
Results: Comparison of the immunophenotype of healthy donor sand mature born kids revealed to decreasing of numbers of CD19+ B cells. Opposite, patients with RP have shown decreased numbers of CD3+, CD4+, CD4+CD25+FoxP3+CD127low T cells and elevated numbers of CD19+ B cells. There were no statistically reliable differences on immunological indicators when comparing children from 1 to 3 months, from 3.5 to 6 months and from 6.5 months to 1 year. Increased symptoms of the disease were followed by increase of B cells (CD19) numbers and statistically reliable decrease of regulatory T cells (Ñ€<0.05), decrease of CD4+ and natural killer cells (CD3-/CD16+CD56+). Evidently, expanded ex vivo autologous Tregs could be used for RP therapy.
Соnclusion: Prematurely born kids with retinopathy demonstrated decreased numbers of peripheral regulatory T cells CD4+CD25+FoxP3+CD127low (Tregs). Tregs play a crutial role in the development of autoimmune diseases, and they can be a cause of complications in retinopathy. The results demonstrate reverse correlations between severe stages of retinopathy in premature born babies and low numbers of regulatory T cells CD4+CD25+FoxP3+CD127low as well as CD4+ and NK cells.
Keywords: Retinopathy of prematurity, cellular immunity, T-regulators, B-cells, immunosuppression, auto-immunity.
Nadezhda V Khamnagdaeva
Pirogov Russian National Research Medical University, Moscow, Russia
Title: Disorders of retinol metabolism in the conceptual field of development of adaptive myopia
Time : 11:15-11:30
Biography:
Khamnagdaeva Nadezda V. – MD, Ph.D., Senior Lecturer of Pathophysiology department of Pirogov Russian National Research Medical University (Moscow, Russia); Ophthalmologist of Ophthalmology Department of Central Clinical Hospital with outpatient health center.
Abstract:
Purpose: To study the ultrastructural features of the sclera in the simulation of axial myopia in the experiment and the reaction of scleral fibroblasts to various concentrations of all-trans retinoic acid.
Methods: 15 experimental 2 month old animal with weight 2,0-2,5 kilogram took a part in our study. To stimulate myopia, into the left internal carotid artery of every animal, catheter (Vasofix Certo 24G) was installed. Within 6 months, 0.5 ml of trans retinoic acid was administered daily at a concentration of 0.06 mg/ml (Sigma-Aldrich, USA) [5]. Clinical refraction was evaluated and echobiometric studies were performed. Transmission electron microscopy was used for morphological studies of scleral samples. Determination of the sensitivity of fibroblasts to retinoic acid was assessed using a microtetrazolium test (MTT test).
Results: The formation of axial myopia is closely related to scleral remodeling. Trans-retinoic acid is a factor that affects on proliferative activity of fibroblasts, hypertrophy and hyperplasia of cells, an increase in the volume of an extracellular matrix, thinning of collagen and elastic fibers.
Conclusion: A model for the formation of axial myopia in which the main initiating factor of pathogenesis is a violation of the process of physiological regeneration of photoreceptor disks is proposed. The slow absorption of retinal pigment epithelium by the cells of distal fragments of photoreceptor disks leads to the activation of oxidative processes (the concentration of vitamin A decreases and the concentration of trans retinoic acid increases). Activation of lipid peroxidation has a damaging effect on cells of the vascular endothelium, the photoreceptor layer of the retina, scleral fibroblasts. Remodeling of the sclera develops with the background of a weakened transfer of necessary metabolites through the damaged endothelium and causes the synthesis of a fragile V type of collagen with short chains.
Kanyukova Gulnara Abdulhakovna
Maternity hospital No. 3, Ufa, Russia
Title: Morphophysiological study of possible ways of delivery of neuromodulators from the retina to the sclera to confirm the hypothesis of the theory of changes in the retinal defocus
Time : 11:30-11:42
Biography:
Abstract:
Background: Today, more and more importance is attached to the research of the ways of extravascular, including interstitial transport of substances, providing the whole complex of metabolic and drainage functions in various anatomical structures of various tissues and organs, including in the eye. On the possible presence of this mechanism, one of the hypotheses in the theory of peripheral retinal defocus is also based, while unconfirmed by clinical studies.
Objective: To detect the transport mechanism, possibly produced by the retina of neurotransmitters, affecting the scleral collagen formation, as well as the physiological ways of their delivery from the vitreous chamber to the sclera. The use of this approach makes it possible to investigate the mechanisms of metabolic processes that can explain the general patterns of transport of metabolites, including the remodulation of scleral collagen in norm and in myopia.
Methods: A method of investigation was used to evaluate the functional activity of interstitial transport paths by introducing color markers and processing the photographs of the obtained frozen slices using the multifractal parameterization method using a special program. The ways of distribution and elimination of color markers of different specific gravity introduced into the vitreous chamber of the rabbit eye with the blood flow and absent in the eye and in models of retinal and choroidal blood flow disturbances were investigated and also the method of investigation from the introduction of magneto-contrast substances into the vitreous chamber of the rabbit's eye and the visualization of their in vivo removal by the means of magnetic resonance imaging.
Results: The data obtained show that for transportation in the eyeball of substances with different molecular weights there are separate ways of their removal from the vitreous chamber. In the peripheral parts of the retina, substances with a lower molecular weight are excreted in the ora serrata region. In the central parts of the retina, substances with a greater molecular mass along the axons of the ganglion cells within the optic nerve migrate. Transport of dyes through the retina and choroid from the vitreous chamber was not detected.
Recent Publications
1. Rodionov O V, Granadchikov V A and Shumkin A M (2008) Influence of disturbance of retinal and choroidal circulation on interstitial transport of chorioretinovitreal interface. Modern technologies of treatment of vitreoretinal pathology. Moscow, 2008.
2. Granadchikov V A, Rodionov O V, Kantukova G A and Bulatov R T (2004) The use of nuclear magnetic resonance tomography in the study of circulation of intraocular liquids in an experiment. Bulletin of the University of Orenburg 234-235.
Masian Janek
North-Western State Medical University after I.I. Mechnikov, Russia
Title: Physiological features of fluid exchange processes in the animal’s eye
Time : 11:42-11:54
Biography:
Abstract:
One of the main problems of modern ophthalmology is the development of a unified concept of the exchange of aqueous humor in the eye. It is generally accepted that aqueous humor circulates mainly in the anterior segment of the eye. However, the involvement of the posterior part in the exchange of aqueous humor eyes is not represented. The purpose of the study is to identify of the mechanisms of water exchange processes in the lens and vitreous chamber of the rabbit's eye. Fluid transport processes in the lens were studied in vitro by the change in mass when immersed in the washing environments of the lenses, with the addition of an inhibitor of the active transport system Na+,K+-ATPase and without it. The direction of movement of aqueous humor was studied in vivo by the displacement of the fluorescein using biomicroscopy and stopped diffusion. The removal of aqueous humor from the vitreous chamber was investigated by changing the concentration of the fluorescein in blood plasma taken from the vascular eye veins and the lateral ear veins, with increased or decreased pressure in the vascular system. It is established that water exchange processes represent the physiological mechanism of breathing in the lens at the moments of accommodation near-in the distance. At a sight in the distance pressure in the flattened lens is minimal; therefore fresh aqueous humor enters the lens through its anterior capsule. The active ion transport system Na+, K+-ATPase, which is localized in the epithelium of the anterior capsule, promotes the osmotic transport of fresh aqueous humor and its further unidirectional diffusion from the anterior capsule to the posterior. Intensive receipt of aqueous humor maximally increases the inside the lens pressure to 6 mmHg and translates the lens into a accommodation phase near. Тhe lens is maximally rounded and the greatest inside the lens pressure, which promotes the diffusion of spent aqueous humor through the posterior capsule. The movement of aqueous humor in the vitreous chamber takes place in the direction of the retina along the gradient of the oncotic pressure. Excretion of aqueous humor from the eye's posterior part occurs through the eye's vertical veins into the total bloodstream. In this way, the first time is presented the theory of the water exchange process at the moments of accommodation near-in the distance, which was confirmed in experiments in the eyes of rabbits in vivo and in vitro. The presented physiological process makes it possible to understand the functioning of the eye in norm and in pathology.
Recent Publications
1. Koschitc I N, Svetlova O V and Gorban' A I Functioning of the executive mechanisms of accommodation and the development of the Helmholtz accommodation theory. Normal physiology of the eye. SPb .: Publishing House of SZGMU them. I. I. Mechnikov.
2. Stepanova L V, Sychev G M and Svetlova O V (2014) Features of water exchange processes in rabbit lenses. Eye 6(100):29-33.
Sidorenko Evgeniy Ivanovich
Pirogov Russian National Research Medical University, Russia
Title: Pathogenesis of retinopathy of prematurity
Time : 11:54-12:14
Biography:
Sidorenko Evgeny Ivanovich - corresponding Member of the Russian Academy of Sciences, Honored Scientist of Russia, Honored Doctor of Russia, Professor, Med.Sc.D., Head of the Department of Ophthalmology of the Pediatric Faculty Russian National Research Medical University by name N.I. Pirogov, Member of the European Society of ophthalmologists, Coordinator of the intergovernmental German-Russian Commission on medicine and the international Alliance of highly developed countries in medicine M8, Founder and editor-in-chief of the Journal "Russian Children Ophthalmology". Author of 668 articles, 27 monographs and 7 textbooks, 56 patents. He has supervised 16 theses Med.Sc.D. and 52 PhD. Scientific activities: perinatal ophthalmology, retinopathy of prematurity, pathology of the visual and nervous apparatus of the eye, hypoxic conditions in ophthalmology, neuroophthalmology, refractive surgery, laser surgery, laser treatments for diseases of the optic nerve and congenital glaucoma. He was awarded the medals of Ehrlich and Albert Koch (2006) for the discovery of infrasonic phonophoresis phenomena.
Abstract:
Despite great success in the study of retinopathy of prematurity, its pathogenesis is not known. The aim of this work is to study the pathogenesis of retinopathy of prematurity. We offer our concept of the pathogenesis of retinopathy of prematurity, based on the result of the studies conducted by our department by Nikolaeva GV, Amkhanitskaya LI, Sidorenko EE. A premature baby that is born is not ready for life in an air atmosphere. The body has two systems providing defense mechanism against hyperoxia and hypoxia; their balance creates homeostasis of the living organism. In the eye of a premature baby a tragedy occurs: two thirds of the retina dies from circulatory hypoxia, and one third - the vascular retina – from hyperoxia. In order to preserve homeostasis, two defense mechanisms activate simultaneously and work in opposition to each other; the system of struggle against hyperoxia and the system of struggle against hypoxia. The dominance of one of them directs angiogenesis in different directions. In our opinion, if hypoxia dominates in the avascular retina then the hypoxia regulating system will be stimulated and angiogenesis proceeds normally in 70-80% of cases. In this case which is the normal pathway, hypoxia leads to an increase in the hypoxic-induced factor (HIF-1a, 1c) which stimulates the production of VEGF, insulin-like growth factor-1 (IGF-1), and placental factor, which causes transaminase blocking and depolarization of vascular walls, increased activity of endothelial cells, and the formation of new vessels. Pathological angiogenesis of retinopathy of prematurity launches a system to combat hyperoxia in the vascular part of the retina which dies due to hyperoxygenation. Immature autoregulation of the vessels in this part of the retina causes pathological angiogenesis. We studied the formation of vascular autoregulation as an important part of the system for controlling hyperoxia in 642 premature infants with a gestational age of up to 30 weeks and weighing up to 1500 grams (Nikolaeva G.V.). It is established that autoregulation is formed only by the 30th week of post-conceptual age. Before this age, oxygen drive reacts inappropriately to oxygen with pronounced angiospasm. Angiospasm develops even at low values of pO2 and normal or borderline with the upper limit of the norm pCO2 (pO2 40-60 mmHg, pCO2 35-45 mmHg), which reflects discoordination in the work of hyperoxic and hypercapnic drives and lead to inadequate protection of tissues from oxygen. The less the degree of maturity of the child, the more often the arteriospasm of the retina is revealed. Births with a gestation period of 25 to 27 weeks showed arteriospasm in 82%, at a period of 28-29 weeks - in 67%, 30-32 weeks - in 54% of cases. In children at the age of 24-25 weeks the caliber of vessels is twice as less than at the age of 30 weeks. The development of retinopathy of prematurity depends not so much an angiospasm itself but rather to its degree, that is, the degree of difficulty in the blood flow. Angiospasm was examined using an index of resistance in the anterior cerebral artery and in the orbital artery. It was found that the greatest difficulty in blood flow caused by spasm of the arteries occurs at the age of 25-26 weeks from conception. The level of the index of resistance of the anterior cerebral artery (IR pm) equal to 0.8 or more indicates a critical obstruction of hemodynamics, the development of a critical level of circulatory hypoxia, which contributes to the release of VEGF. During the retinopathy of prematurity, a large part of the retina without oxygen is suffocating, and hyperoxygenation in a small segment of the eye with blood vessels destroys the hypoxic inducing factor and blocks the work of the system for controlling hypoxia. Alpha HIF1 is extremely unstable to oxygen and undergoes its degradation under aerobic conditions. This delays angiogenesis and circulatory hypoxia gradually becomes total in the vascular and avascular retina, the hypoxia zone expands, and the hypoxic inducing factors HIF1.2,3 begin to accumulate with a large delay and the angiogenesis system starts. The second problem is the delay of angiogenesis and the prolonged period of hypoxia which leads to the growth of spindle and glial cells of the retina in the form of a shaft that directs the growth of the newly formed vessels into the vitreous (intravitreal). And here there is a third problem, established by us (Akhmanitskaya LI), the first phase of retinopathy of prematurity is the oxygen aggression of the vitreous body on the retina, which stimulates the work of the system for controlling hyperoxia. Oxygen accumulates in the vitreous as in the depot and continues to affect the retina within 6 hours after the cessation of its inhalation. All this causes the pathological angiogenesis in the second acute stage of PH.
Svetlova Olga Valentinovna
North-Western State Medical University named after I.I. Mechnikov, Russia
Title: About the possibility of another diagnosis of glaucoma and age ocular hypertension using a pneumatic analyzer ORA by criteria of rigidity and fluctuation of the scleraSvetlova Olga Valentinovna
Time : 12:14-12:29
Biography:
Olga V. Svetlova, Med.Sc.D., professor of Department Ophthalmology of North-Western State Medical University named after I.I. Mechnikov. She is the author of 211 scientific works, 2 monographs (2016). More than 25 years, she has been conducting research on Biomechanics and physiology of the eye at the intersection of academic disciplines. The co-author generalized classification of executive mechanisms of accommodation and proposals for development of the theory of accommodation of lens by Helmholtz, including the joint work of the front mini-lens and posterior mini-lens in the capsule of the lens to create a sharp image. She is the co-author and developer of the theory of functions of fibrous sheath eyes, the theory of open angle glaucoma and metabolic adaptation theory of acquired myopia; as well as the co-author of new dynamic diagnostic methods to determine the in vivo new physiological and biomechanical characteristics of the eye.
Abstract:
Introduction: The issue of diagnostic division of age-related ocular hypertension (AOH) and open-angle glaucoma (OAG) today is one of the most important questions in practical ophthalmology. AOH is not actually a disease and is physiologically necessary to maintain intraocular metabolism with age. AOH is a physiological response of the eye to the gradual aging process of its structures, which leads to a continuous smooth increase in rigidity of the sclera, a decrease in its permeability and a gradual response to the growth of intraocular pressure (IOP). Similarly, arterial hypertension develops due to increased vascular rigidity. However, the classical OAG is a pathological condition, when the aging of the eye structures is ahead of the usual aging. The aging processes of the eye at OAG become abrupt: the rigidity of the sclera increases sharply by 1.5-3 times, in response IOP grows abruptly [1-3]. The practical physician is often experiencing significant difficulties with the diagnostic attempts to distinguish AOH from OAG. After all, reliable IOP means for healthy eyes with AOH and standards for eyes with OAG are not actually developed. Until recently, it was not even possible to determine which range of the true IOP norm belonged to the patient's eye at a young age: low (9-12 mmHg), average (13-16 mmHg) or high (16-22 mmHg). Therefore, the doctor is often forced to use the mythical "average pressure in the hospital", prescribing treatment without taking into account the rate of true IOP in young patients. In addition, there are no baroreceptors in the eye, so the eye does not control the pressure, but controls its volume with the help of mechanoreceptors and prostaglandin receptors of the sclera [4,5]. For a number of objective reasons in the conditions of evidence-based medicine archaic criterion of "IOP level" is no longer reliable [2,3,6]. For example, the levels of IOP in AOH in the eyes of the high-range IOP in youth or in the eyes of early stage OAG with low-range standards of IOP in youth, IOP can often be the same, although changes in the visual field and excavation of the optic disc would not be detected. And it is almost impossible to distinguish AOH and OAG from each other by means of traditional differential diagnostics. As a result, the doctor is often forced to prescribe antihypertensive drugs in both cases. However, pathogenetically poorly justified reduction of IOP in the eye by any of the known methods by 20, 30 or 40% worsens the metabolism of intraocular structures, accelerates their aging and creates prerequisites for the transition of AOH to OAG. In fact, we are using traditional methods of treatment to accelerate the transition of AOH to OAG, as well as the progression of OAG into developed stages. To reverse these negative trends new methods of differential diagnosis and treatment will need to be developed and implemented.
Material and Methods: The first group consisted of patients with AOH under the age of 75 years, a total of 326 healthy eyes with a high-range of IOP in youth. The second group consisted of patients aged 55-76 years with primary OAG, a total of 75 glaucomatous eyes with a low-range of IOP in youth. The level of current true IOP in both groups at the time of the examination was 23-28 mmHg For the differential diagnosis we used the modified pneumatic analyzer ORA, whose computing platform was thoroughly upgraded [1,3,7-8]. This allowed the Koshits-Svetlova method to determine in vivo the volumetric rigidity of the fibrous sheath of the eye (FSE), the true IOP according to Goldmann, the IOP level in youth, the belonging of the eye to the low-range, average, or high-range IOP rates, as well as the parameter introduced by us – scleral fluctuation (SF) [1-3,5,7-10]. In Pic. 1 the scheme shows measurement of physiological parameters of FME using our technique. SF is a new functional parameter in ophthalmology, which characterizes the ability of the sclera to restore its original shape after the pneumatic impact. SF also characterizes the functional ability of F to directly participate in the outflow of intraocular fluid, due to the retaliatory reduction of the internal volume of FSE with the help of pre-stretched elastic collagen fibers of the sclera and myofibroblasts.
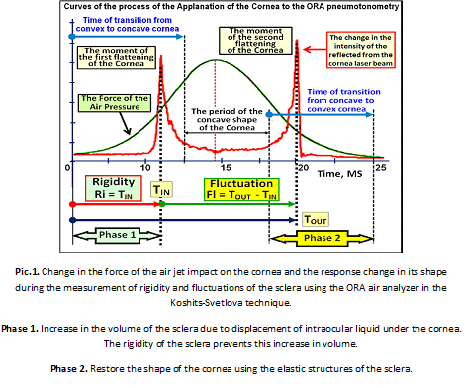
Results: The increase in rigidity and decrease in scleral fluctuation with age are presented in table 1. A comparison of the values of the rigidity of FSE in healthy and glaucomous eyes within a close age group reveals significantly higher level of stiffness in glaucomous eyes than in healthy and, consequently, a lower level of fluctuations of the sclera (Pic.2).
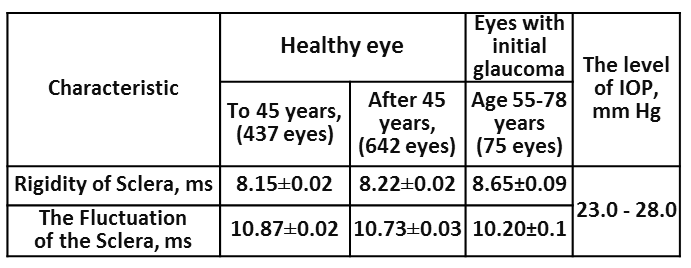
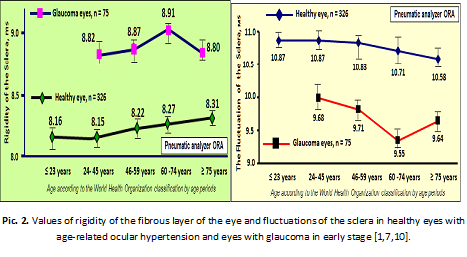
In the eye with OAG age-increased rigidity of the sclera superimposes the processes of accelerated aging of FSE, which leads to abrupt jump in rigidity and a significant reduction in the functional capacity of the sclera to fluctuate. This significantly reduces viscoelastic and functional properties of FSE in general. Moreover, the level of FSE rigidity in the glaucomatous eye already in the early stages of OAG significantly exceeds the levels of rigidity compared to healthy eyes with AOH in the elderly. But the most important thing is that the regions of finding representing the rigidity and fluctuation (Pic. 2) for AOH and OAG do not intersect anywhere. This allows reliably and objectively diagnose AOH or OAG separately from each other.
Discussion: It became clear that the development of norms/standards of rigidity and fluctuation of the sclera for healthy and glaucomatous eyes from the point of view of the physiology of the eye is much more effective than the development of standards for uncontrolled levels of IOP in the eye. After all, the fluctuation and rigidity directly characterize the current functional state of the FSE, which must be maintained independently if this is the prevention of AOH or the treatment of OAG. So restoration or maintenance of functional fluctuations of the sclera is pathogenetically justified method of treatment of the OAG or prevention of the AOH. This will ensure functional state of intraocular exchange of aqueous humor by maintaining the level of scleral fluctuation not less than 50-60% of the norm. Targeted reduction of rigidity of the sclera or the current IOP must ensure the maintenance of the scleral fluctuations at physiologically reasonable level [11,12].
References
1. Svetlova O. V., Koshits, I. N., Ryabtseva A. A. et al. The Role rigidity of the fibrous layer of the eye and fluctuations of the sclera in the early diagnosis of open-angle glaucoma.-Ophthalmol. Journal, 2010.-6:76-88. [in Russian, in English].
2. Svetlova O. V., Ryabtseva A. A., Koshits, I. N., Makarov F. N., Guseva M. G., Zaseeva M. V. About selecting effective strategies and tactics in the early diagnosis, prevention and treatment of open-angle glaucoma. Part 1. Status of the issue and assumptions.- Ophthalmol. Journal, 2014. - 2 (457): 118-133. [in Russian, in English].
3. Svetlova O. V., Ryabtseva A. A., Koshits, I. N., Makarov F. N., Guseva M. G., M. V. Zaseeva. About selecting effective strategies and tactics in the early diagnosis, prevention and treatment of open-angle glaucoma. Part 2. Theory and practice. New medical technology.- Ophthalmol. Journal, 2014. - 3 (458): 104-118. [in Russian, in English].
4. Vit V. V. The Structure of the human visual system.- Odessa, Astroprint.- 2003.- 655 P. [in Russian].
5. Svetlova O. V., Drozdova G. A., Balashevich L. I., Zaseeva M. V., Ryabtseva A. A., Makarov F. N., Koshits I. N. Morphological and physiological features of the structure of the sclera of the human eye as a key element in shaping the level of intraocular pressure in normal and glaucoma.- Morphology.- 2009.- Vol. 136.- (5): 5-10. [in Russian].
6. Gorodnjanskaja E., Svetlova O., Makarovskaia O., Pankratov R., Koshits I., Makarov F. Low confidence of the IOP criterion and clinical efficacy of OAG diagnostic by sclera rigidity and fluctuations levels and by IOP value in the youth.- 7th World Glaucoma Congress: Abstract book, 2017.- Helsinki.- P. 505.
7. Svetova O. V. Functional features of interaction of sclera, accommodation and drainage systems of the eye in glaucoma and myopic pathology. ...Diss. doctor of medical science-M., 2010.- 186 p. [in Russian].
8. Zaseeva M.V. Study of the rigidity of the sclera in healthy and glaucoma eyes.- Diss. PhD.- Military Medical Academy.- Saint-Petersburg.-2009.- 145 P. [in Russian].
9. Svetlova O. V., Koshits I. N. Physiological functions of the fibrous membrane of the eye and their Executive mechanisms. Normal and pathological physiology of the eye: monography. – Saint-Petersburg: House of North-Western State Medical University by name I. I. Mechnikov, 2014. - 64 p. [in Russian].
10. Svetlova O., Koshits I., Guseva M., Makarov F. Two key managers in the pathogenesis of OAG and innovative methods of early diagnosis.- 7th World Glaucoma Congress: Abstract book.- Helsinki, 2017.- P. 532.
11. Svetlova Olga, Koshits Ivan, Drosdova Galina. Interaction mechanisms outflow and accommodation for myopia and glaucoma. Pathophysiology: monography. -2 Edition.- St. Petersburg: Northwestern State Medical University by name I.I. Mechnikov, 2016.– 164 Ñ€. [in Russian].
12. Alla Ryabtseva, Sergey Sergushev, Roman Pankratov, Ivan Koshits, Olga Svetlova. Non-penetrating laser hypotensive sclerectomy as an alternative method of OAG treating at last stages.- 7th World Glaucoma Congress: Abstract book.- Helsinki, 2017.- P.526.
Yugay Maria Pavlovna
The Moscow regional research clinical institute of. M.F. Vladimirsky, Moscow, Russia
Title: Changes of intraocular pressure and cornea biomechanical properties after cataract phacoemulsification
Time : 12:29-12:41
Biography:
Maria Yugay, PhD, graduated with honours Kuibushev Medical Institute n.a. D.I.Ylianov (1989). She is an ophthalmologist, works in Moscow regional research clinical institute of M.F. Vladimirsky.
Abstract:
Purpose: Cataract phacoemulsification is accompanied by changes in intraocular pressure and biomechanical parameters of the eye. Our purpose was to analyze the changes of intraocular pressure and corneal hysteresis during 3 months after phaco.
Methods: The study included 80 eyes of 80 patients who underwent uncomplicated phacoemulsification through clear corneal incision with IOL implantation. Preoperative examination included standard techniques and measurement of corneal hysteresis, central corneal thickness (CCT), corneal compensated intraocular pressure (IOP) and Goldman IOP by ocular response analyzer, repeated before surgery, 1 day, 2 weeks, 1 and 3 months after surgery.
Results: Corneal hysteresis decreased on the first day after cataract phacoemulsification from 9.90±0.24 mmHg to 8.88±0.26 mmHg and after 2 weeks to 7.91±1.13 mmHg (p<0.05). Then corneal hysteresis started to increase and after 3 months after surgery returned to preoperative values (9.78±0.29 mmHg). Intraocular pressure increased after surgery by 3 mm Hg, decreased to preoperative values by 1 month after phaco, and continued to decrease by 1.5-2 mmHg up to 3 months after phacoemulsification
Conclusion: Corneal hysteresis decreased in the early postoperative period after phaco, dropping to a minimum 2 weeks after surgery. Then corneal hysteresis gradually increased, reaching preoperative values at 3 months after surgery. Changes of intraocular pressure are opposite to changes of corneal hysteresis. CCT increased after phaco, reached maximum in 2 weeks and returned to preoperative values in 3 months.
Khalimova Liliya Ilusovna
Pirogov Russian National Research Medical University, Moscow, Russia
Title: Modification of biomechanical properties of cornea with different UV corneal cross-linking protocols ex vivo
Time : 12:41-12:53
Biography:
Azat R. Khalimov, B.Sc.D., Head of Research and Production Department of Ufa Eye Research Institute, The author of 1 monography, 170 research papers, 30 patents of the Russian Federation and 2 innovation proposals. More than 10 years, conducts research on UV corneal cross-linking. Is a developer of devices and medicines for UV corneal cross-linking. Research interests: ophthalmology, UV corneal cross-linking, pathological physiology, biophysics, biochemistry.
Abstract:
Aim: Collagen cross-linking (CXL) with UV-A irradiation 370 nm and 0.1% riboflavin stabilizes the pathological process in the cornea. Improvement of the Standard UV-A corneal cross-linking resulted in Accelerated and Pulsed-light accelerated UV-A cross-linking. It is necessary to compare these UV cross-linking techniques to assess its efficacy.
Methods: The experiments were carried out on 36 porcine eyes in 4 groups (8 porcine eyes each) ex vivo: 1st group – intact (control); 2nd group – standard UV-A corneal cross-linking (S-CXL) – 3 mW/cm2, 30 min; 3rd group – accelerated UV-A corneal cross-linking (A-CXL) – 18 mW/cm2, 5 min; 4th group – pulsed-light accelerated UV-A corneal cross-linking (Pl-A-CXL) – 18 mW/cm2, 10 min, pulsed exposure (1 sec on / 1 sec off). In all experimental groups Epi-Off, UV-A light 370 nm and 0.1% Riboflavin + 20% Dextran was used. The flaps from the cornea were stretched until they were completely ruptured using a universal tensile testing machine. Biomechanical properties were assessed by the force at rupture and the Young's modulus.
Results: All investigated methods of UV-A cross-linking led to an increase in the force at rupture and the Young's modulus of the porcine corneas. Young's modulus increased: S-CXL by 98 ± 12,1%, A-CXL – 86 ± 9,4% and Pl-A-CXL – 89 ± 10,2%. Ultimate tensile strength increased: S-CXL by 67.8 ± 9.5%, A-CXL - 55.3 ± 7.2%, Pl-A-CXL - 58 ± 8.1%. The maximum results of biomechanical strength were obtained in the S-CXL group. However, statistically significant difference between Standard, Accelerated and Pulsed-light accelerated UV-A corneal cross-linking was not obtained.
Conclusions: Standard, Accelerated and Pulsed-light accelerated UV-A corneal cross-linking increased the biomechanical properties of porcine corneas ex vivo and Young's modulus. Standard UV-A corneal cross-linking had slight advantage.
Kaptsov Valery Alexandrovich
All-Russian Scientific Research Institute of Railway Hygiene, Russia
Title: Illumination in educational institutions and the vision of students
Time : 13:53-14:08
Biography:
Valery A. Kaptsov. In 1987 defended the doctoral dissertation,and in 1988 was appointed deputy director of the Russian Academy of medical sciences (RAMS) institute of occupational health. From 1993 to 2005 worked as the director of the All-Russian Research Institute of Railway Hygiene. In 2004 was elected associated member of RAMS, in 2014 - associated member of Russian Academy of sciences. From 2005 to 2013 - Deputy Director of the Institute. From 2013 - Head of the Department of Occupational Health the same Institute. He has published more than 500 papers in journals and has been serving as an editorial board member.
Abstract:
In 2014, the World Health Organization (WHO) published statistics according to which about 285 million people suffer from visual impairment; 246 million of them have low vision. The most common cause of disease (43%) is uncorrected refractive errors, including myopia. F. F. Erisman pointed out "I must add that myopia is not an inevitable evil that must be associated with school education; on the contrary, progressive myopia is an evil that arises only from the inappropriate device of schools, and this evil would, of course, be eliminated if the device of schools would be drawn to the attention of society." In schools in China to combat myopia modified Erisman's desks limiters that would head students did not fall less than 30cm. At the same time, a stochastic relationship was established between the growth of myopia and the introduction of energy saving light sources with biologically inadequate radiation spectrum. The researchers believe that the fact of long stay inside the premises is the main cause of the problem, which after the elimination of other factors, is reduced to the effect of light on the development of myopia. Sergey Vavilov noted that from the biological point of view," optimal illumination» should be the result of evolutionary adaptation of the eye to the average illumination created by the Sun. The eye in relation to energy is not adapted to the Sun itself, but to the sunlight scattered from the surrounding bodies. Modern people began to spend much less time on the street, and this provokes the appearance of myopia, since under the influence of bright daylight the retina of the eye produces dopamine and controls the diameter of the pupil of the eye, and its lack and causes the elongation of the eyeball. When assessing the productivity and fatigue in the light of an incandescent lamp, mercury and fluorescent lamp, the following is established.
To create equal levels of productivity and fatigue need lighting:
- incandescent lamps 300 lux;
- fluorescent lamps – 500 lux (above 1.66 times than that of incandescent lamps).
In the evaluation of visual performance when
natural and artificial lighting is set as follows.
At equal levels of visual performance for :
- natural light desired illuminance 300 lux;
- artificial lighting - 500 lux (1.66 times higher than for natural lighting).
Schools generally use combined lighting (sunlight plus energy-saving lamps).
The spectrum of combined lighting is characterized by high unevenness, increased dose of red light in comparison with the spectrum of sunlight and violated the law of optimal control of the pupil diameter of the eye and ATP synthesis, which increases the risk of myopia and ADM.
Summary
1. The study of the biological effects of light on humans is an urgent problem of lighting hygiene. Biological inadequacy of natural and artificial light of equal intensity, experimentally proved at cellular, biological and psychophysiological levels, is maintained even with increasing light level from artificial sources.
2. The hygienic value of natural light must be taken into account when developing lighting standards and new artificial light sources for long-stay rooms.
3. The increase in the level of illumination of artificial light sources by 1.6-2 times compared to natural light contributes to the preservation of a high level of productivity and visual performance, but does not solve the problem of reducing myopia during prolonged work in artificial lighting.
4. When combined natural and artificial light occurs uneven spectrum of radiation, different from the spectrum of sunlight, which increases the risk of myopia.
Recommendations:
1. For the optimal functioning of the visual analyzer and the human hormonal system, it is necessary to introduce semiconductor light sources with biologically adequate radiation spectrum.
2. Implement the recommendations of the 3rd Global Pediatric Congress, held in March 2018 in London to improve the coverage of educational and medical institutions.
Andryukhina Anna Sergeevna
Moscow Regional Research Clinical Institute of M F Vladimirsky, Russia
Title: The theoretical background for invention of preventive light protection glasses at an early stage of AMD
Time : 14:08-14:23
Biography:
Anna S Andryukhina has completed her graduation from Russian National Research University of N I Pirogov in 2016. She is an Ophthalmologist, working as a Doctor in Moscow Regional Research Clinical Institute of M F Vladimirsky, Russia.
Abstract:
There was a medical-biological study about advantage of preventive light-filter glasses with the initial age-related macular degeneration (AMD). The main idea is based on selective light diminution in the spectral band of rod sensitivity with a relatively high transmission in the bands of conical day vision. An important factor in the progression of AMD in the initial period is increased generation of free radicals in RPE cells. Molecules that produce free radicals are bis-retinoids: derivatives of free retinal released during the decolorization of rhodopsin. The most massive supplies of free retinal in the retinal pigment epithelium (RPE) occur as a part of the phagosome of the external segments of the retina rods. The possible cone component appears to be insignificant because of the low content of conical visual pigments in the retina in comparison with rodopsin of the rods. The most significant discoloration of rhodopsin rods and release of free retinal occurs due to daylight. At the same time, in the daylight visual information is provided by cone vision, while the rods are not involved in the visual process. This situation opens the technical possibility of creating preventive light-filtering AMD-glasses for the elderly. Spectral calculations of this type of optical filters have shown the theoretical possibility of 100-1000 fold weakening of the fading of the rhodopsin-filled rods, while maintaining a full-fledged day vision in the conditions of daylight illumination. Experimental samples of such light filter glasses were prepared and tested. In biological studies on the suspension of the external segments of the retina rods of experimental animals was shown the possibility of multiple selective attenuation of the fading of rhodopsin of the rods while using this glasses. Optometric studies revealed that in conditions of high daylight illumination ( >10,000 Lk) these glasses do not reduce visual acuity with the preservation of normal trichromatic color perception with a general high visual comfort.
Koshits Ivan Nikolaevich
Petercom-Network Management System/Consulting Grope Close Corporation, Russia
Title: Optical features of the anterior segment of the eye and lens
Time : 14:23-14:35
Biography:
Ivan N. Koshits is mechanical engineer, biomechanics, a member of the St. Petersburg Sechenov Society of physiologists, biochemists, pharmacologists. Author of 70 scientific works in biomechanics, normal and pathological physiology of the eye and its elements, 2 monographs (2016). Organizer and co-head of the first scientific conferences in Russia on the Biomechanics of the eye in 1998 -2009. Author dispersion theory aiming eye on sharpness and formation mechanisms of binocular vision due to optical rings-sights in the macula. Co-author and developer of the theory of functions of fibrous sheath eyes, the theory of open angle glaucoma and metabolic theory of adaptation myopia. As well as the co-author of dynamic diagnostic methods to determine the in vivo new physiological and biomechanical characteristics of the eye. General Director of the company of Petercom - Network/Management System Consulting Grope Cl. Corp.
Abstract:
1. Optics of the anterior segment of the eye. We are used to idea that light rays entering the eye are refracted by the cornea. However, this is not the entirely true. Incoming light rays first pass through the first barrier: the tear film with the epithelium, where the refractive index (RI) = + 43.6 D on the border with air. And only then the rays pass through the second barrier "tear film – cornea" with RI = + 5.3 D. There is no air layer between the epithelium and the cornea, which makes it possible to create a kind of biological optical system: "tear film + epithelium + cornea". Such optical design of anterior segment of the eye produces a kind of" optical compression", it "collects" a wide picture of the visual space in the eye in a narrow" optical tunnel", as in a telescope. This optical compression is necessary in order to provide the possibility of passing the light bundle even through a narrow pupil (Pic. 1).
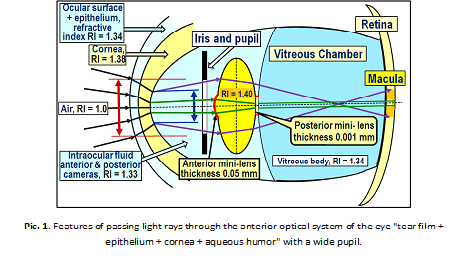
The thickness of the cornea in the center is almost 2 times less than in the periphery, which is typical for the scattering lens. Therefore, for example, the white light rays coming out of the cornea at the border of the "cornea – intraocular fluid" will be slightly divergent (see Fig. 1) and further subject to dispersion, decomposing into a spectrum, this means that inside the eye there will always be rays of all colors of the spectrum and only in the center of the cornea wavelengths of light will all be in one bundle – the white light. Furthermore, the anterior optical system (AOS) of the eye, consisting of the "eye surface" and the cornea, borders with a less dense optical medium – intraocular fluid. AOS works as a biological lens, providing at first compression in the "light tunnel", and then - a weak scattering of passing light rays.
Therefore, white light rays will always be subject to dispersion on the posterior surface of the cornea, and will go to the anterior surface of the lens as slightly divergent and expanding color bands, including three base bands: blue, green and red (BGR-band), which can be detected by macular cones. The effect of thickness and topography of the tear film with corneal epithelium on the overall refractive power of the eye is quite noticeable. Therefore, in dry eye syndrome, patients often complain about the lack of image sharpness, since the thinning of the lacrimal surface significantly reduces its refractive power.
2. Optical structures of the lens. The mystery of the focusing mechanism of light rays that pass close to the optical axis of the eye exactly into the macula for many years had no solution. Traditionally, it was believed that the lens capsule cannot strongly refract light in its central region due to the small curvature radius. As it turned out, this is not a complete picture. In the center of the anterior and posterior surfaces of the lens capsule there are two thin mini-lenses: the front mini-lens and the rear, which change their optical powers depending on the pressure inside the lenses capsule, depending on the tone of the ciliary muscle (Pic. 1). These mini lenses provide maximum refraction when looking at the objects at the minimum distance. Pic. 2 shows the change in the geometry of the front and rear mini-lens in the extreme phases of accommodation. When looking at closely located objects the pressure in the capsule of the lens is as big as its refractive power (the circumference) of these mini-lenses. When looking into the distance, the pressure inside the lens bag same as the refractive power of the mini lenses are at its minimum. This is because when you look objects placed at near distance the capsule of the lens is the least stretched by the ciliary zonules and therefore the most powerfully compresses structure inside the lens.
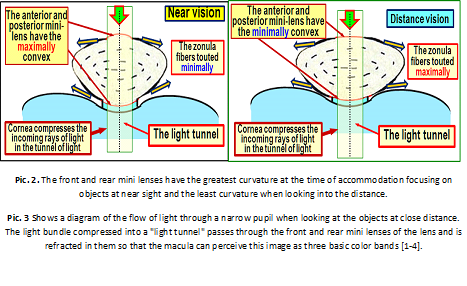
Conclusion. The anterior optical segment of the eye is a composite biological lens, which includes the following refractive structures: tear film, corneal epithelium and the cornea itself. The main task of the eyes optic system is to effectively compress into a "light tunnel" with a diameter of 1.8 -2.5 mm coming into the eye light flux for it to pass even through the narrow pupil. The cornea is a weakly scattering lens, so the light rays are spread out in the spectrum at the border with the aqueous humor of the anterior chamber, then undergo a weak deviation from the outside on the posterior surface of the cornea. In the center of the optical axis in the lens capsule there are two mini-lenses – anterior and posterior, which change their curvature (refractive power) in different phases of accommodation due to changes in pressure inside the lens with different tone of the ciliary muscle.
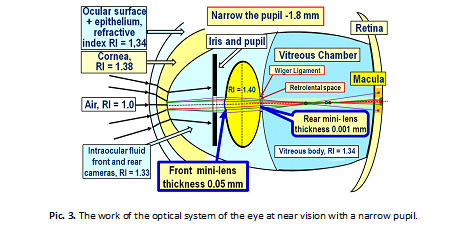
Guseva Marina Gennadievna
Diagnostic Medicine Centre “Vodokanal SPb†Moscow, Russia
Title: The use of features of physiology and optics of the eye in rational optical correction
Time : 14:35-14:50
Biography:
Marina G. Guseva is an ophthalmologist of the highest qualification, optometrist, and experience 30 years. From 2003 to 2011, she was the main ophthalmologist of the Close Corp. "Neva Optics Holding". Since 2011, she was the main ophthalmologist of the Close Corp. "Sfera". Since 2012 she became the Head Doctorophthalmologist in the Medical–Diagnostic center "Medical center "Vodokanal of St. Petersburg" and Close Corp. "The Doctor Lenses SPb". She has 9 international certificates in Optometry: The Vision Care Institute of Johnson & Johnson, Academy for excellence Eyecare Ciba Vision, Easy to adapt to University. In clinical work uses all modern methods of diagnosis of eye pathology. Author of 28 publications, co-author of two chapters in the book "Ophthalmo-contactology" (St.-Petersburg: Military Medical Academy, 2012, 562 p.), one monograph. She is the co-author and developer of a modern method of rational optical correction. For 7 years of research conducted clinical testing and confirmed the performance of Koshits-Svetlova Metabolic theory of adaptive myopia in 2500 patients using all types of modern correction. Her research interests are glaucoma, refractive errors and their combination. She is post-graduate student of Department of ophthalmology, Mechnikov North-Western State Medical University.
Abstract:
Introduction: Traditionally, it is believed that the optical path of the eye has been studied thoroughly and does not require serious research. However, there are still a lot of "uncomfortable" questions that have not been answered. In particular, until now it was unclear the following:
 How do the side light rays get to the periphery of the lens and refract with contracted pupil, and are not blocked by the iris;
 How can light rays, located near the optical axis of the lens, be refracted, despite relatively small curvature of the anterior and posterior surfaces of capsule compared to the periphery;
 Where does white light dispersion occurs – inside the cornea or on the posterior surface of the cornea;
 What type of optical signal coming into the retina macular cones can detect - circles or light scattering bands of blue, green and red (BGR-bands);
 How does the system of "binocular guidance" of both eyes and their individual "optical aim» work in particular;
 What contribution does the cornea, which is a weakly scattering lens, make to the "assembling" optical system of the anterior segment of the eye;
 What should be considered the focus of the eye when it is impossible to simultaneously combine the foci of three wave BGR- fronts on a common focal plane due to the presence of optical axial aberration;
 Which highly reliable optical signal should form the accommodation mechanisms in the macula so that the brain can "track" the moment of accurate eye guidance on the allocated space or adjust the subject sharpness;
 What parameters of BGR-bands formed by the optical system of the eye should be able to fix the macula in general and its fovea in particular to form a feedback signal in the brain to control the ciliary muscle and the accommodation system as a whole;
 How, for example, changes the topography and the refractive power of the cornea by wearing orthokeratologic lenses (OK-lenses), and "optical turning-off" of which physiological adaptational mechanisms of OK-lenses are the most effective in dealing with acquired myopia.
Many unresolved issues in the optics of the eye are still the main obstacle in the creation of adequate laws of optics and mechanics of the theory of accommodation and working theory of myopia. The incremental-retinal defocus theory, which is quite popular today, is controversial, and its hypotheses often do not have a clear morpho-physiological basis [1]. And it is not possible to correctly carry out the correction of refractive disorders. It also became clear that weak understanding of the main features of the optical part of the visual tract of the eye, including the electrical part, stands in the way of creating more effective means of optical correction [1-4]. It is necessary to admit that the theory of optometry for now is poorly developed.
New theoretical and practical results: New executive mechanisms necessary for obtaining image sharpness due to the formation of an optical signal on the retina that is adequate to its physiological capabilities have already been identified [3,4]. Proposed in 2001 Koshits-Svetlova metabolic theory of adaptive myopia proved to be efficient and has already successfully passed clinical confirmation with follow-up periods of 3.5 and 7 years [5,6]. It became clear that a rational optical correction is needed, which uses a weak correction for the far sight, as well as a full correction or a weak correction for work at close range. This allows you to turn off the physiological adaptation mechanism of adjusting the length of the eye under visual load. In fact, this strategy implements OK-lenses. Rational correction is necessary in order to maintain a certain tension of ciliary muscle and with the aqueous humor to provide the transfer via the uveoscleral path a sufficient amount of ingredients for proper metabolism of the collagen structures of the middle and posterior part of the sclera to prevent the elongation of its posterior pole.
Our development of the theory of Helmholtz accommodation led us to understanding that in all phases of accommodation the lens is preloaded with a powerful front portion of fibers to the vitreous chamber (VC). The fibers of the cilliary zonule (CZ) are maximally stretched when looking into the distance and weakened (not relaxed!) when you look at near [7]. This allows the lens bag to be rounded as much as possible and more powerfully compress the intralenticular masses when looking at close distance (Pic.1). Pressing the lens to the vitreous chamber with the help of CZ fibers is carried out in all phases of accommodation and allows such a damping mechanism not only to securely hold the lens in the eye, but also to extinguish its oscillations under inertial loads.
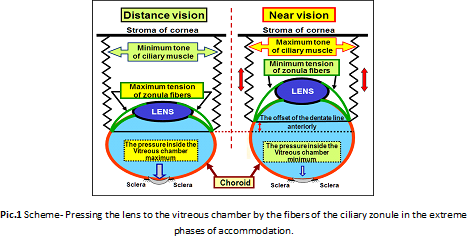
Discussion: These theoretical ideas lead to important practical conclusions. In the case of appointment for the eye with acquired myopia optical under-correction for the ciliary muscle (CM) when looking into the distance and at medium distances is fully or partially relaxed and the amount produced by its processes of watery moisture is significantly reduced. This can significantly reduce the amount of ingredients delivered for normal intralenticular metabolism. There are significant prerequisites for the accelerated development of cataracts in myopic eyes with such irrational optical correction. For example, when looking into the far distance, the amount of intraocular fluid that is produced by the processes of the ciliary body is reduced three times compared to the sight at near, since the CM receives three times less blood [6].
For glaucomatous eyes in combination with myopia it is also very important to avoid under-correction of myopia, since relaxation of CM leads to an increase in pressure in the vitreous chamber, which in some cases provokes a jump in the magnitude of the optic disc excavation and increases the deformation of axons (Pic.2) [8].
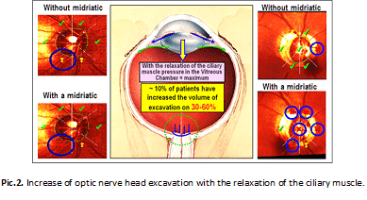
In addition, the open angle glaucoma (OAG) in developed stages the uveoscleral outflow pathway (USOP) is already up to 80% of the total production of intraocular fluid (IF). However, with under-correction, the effectiveness of USOP significantly decreases, which disrupts the metabolism of intraocular structures and leads to an acceleration of their aging processes. Therefore, optical under-correction cannot be used for OAG.
On the contrary, it is advisable to apply a weak rational correction of 0.12-0.25 D in myopia for far sight distance, which will lead when working at medium and long distances to the tone of the CM, close to the average, when the production of IF in the processes of the ciliary body is normal. This is favorable for normal nutrition of the lens, and physiological conditions for accelerated development of cataracts do not occur. In addition, the pressure in the vitreous chamber with such optical correction is not at its the maximum, which reduces the optic nerve head excavation in the OAG. Therefore, it is advisable to use a weak correction to ensure vision in the distance for any refraction.
It is especially important in pair eyes with different refraction to perform a rational optical correction in such a way that both eyes have the same values of residual weak correction to ensure effective binocular work of both eyes. But the most important thing in the art of rational correction - is to provide the possibility of full implementation of the functional range of the ciliary muscle in its normal state to ensure the restoration (manifestation) of the entire physiological volume of accommodation.
Now we should consider the cases of providing comfortable vision at near distance. And here we need to solve two problems: to ensure the normal flow of metabolism in the lens and in the structures of the middle and posterior parts of the eye to prevent the development of cataracts, myopia or dystrophic changes in the retina with high myopia. To do this, it is necessary to "turn off" the usual executive mechanisms of adaptive selection of eye length under increased visual load. To be exact, with the help of competent optical correction, it is necessary to bring the tone of the CM to a state close to the average, which we have long defined as a "pre-installation of accommodation" [5,6]. This we denote as the concept of «optical control of the outflow».
Physiologically this can be achieved with a weak under-correction of 0.5-0.75 D for the near sight in the eyes of any refraction prolonged intensive work in close proximity (e.g., display). After all, with long-term «display visual loads», reaching the residents of megacitys from 5 to 12 hours a day, of course, there will be functional fatigue of СM, which in many developed countries has long been classified as a disease and is equivalent to an insured event. We are talking about computer vision syndrome (CVS). For its prevention, there is only one effective way – rational optical correction or preventive glasses for the near, and, we emphasize - even for healthy eyes. It is clearly necessary to take the next step and move massively to the usual and mandatory preventive correction, given the speed "myopia pandemic" spreads.
References
1. Koshits I.N., Svetlova O.V., Guseva M.G., Balashevich L.I., Makarov F.N., Egemberdiev M.B. Adaptive myopia. Part 1. Actuating mechanisms of optic axis growth in the incremental retinal defocus theory.- Ophthalmic journal,2016.- 6 (473): 45-58. [in Russian, in English].
2. Guseva M.G., Svetlova O.V., Koshits I.N. Stabilization of the acquired myopia in children with the aid of contact lenses from the standpoint of the metabolic theory of myopia.- Ophthalmic journal, 2011.- 6 (443): 29-36. [in Russian, in English].
3. Koshits I.N., Svetlova O.V. Adaptive myopia. Part 2. New views on the physiological mechanisms of the guidance of eyes to sharpen.- Ophthalmic journal,2017.- 1 (474): 38-50. [in Russian, in English].
4. Koshits I.N., Svetlova O.V. Adaptive myopia. Part 3. New mechanisms aiming to sharpen the eyes and their interaction with the mechanisms of the development of acquired myopia.- Ophthalmic journal,2017.- 2 (475): 36-57. [in Russian, in English].
5. Koshits I.N., Svetlova O.V. A mechanism of formation of the eye adequate length in the norm and metabolic theory of pathogenesis of acquired myopia.- Ophthalmic journal, 2011.- 5 (442): 4-23. [in Russian, in English].
6. Koshitc Ivan, Svetlova Olga, Guseva Marina. Physiological principles of rational optical correction. Practical recommendations. Normal physiology of the eye. Tutorial.- St. Petersburg: Northwestern State Medical University by name I.I. Mechnikov, 2016. - 152 Ñ. [in Russian].
7. Olga Svetlova, Ivan Koshits. Theory. Actuating mechanisms of accommodation and development of the theory of accommodation by Helmholtz.- Proceedings of 3rd Global Pediatric Ophthalmology Congress, 2018.- London, UK.- Journal of Clinical & Experimental Ophthalmology, March 2018.- Vol.9.- P. 66-70.
8. Svetlova O., Koshits I., Guseva M., Makarov F. Two key managers in the pathogenesis of OAG and innovative methods of early diagnosis.- 7th World Glaucoma Congress: Abstract book.- Helsinki, 2017.- P. 532.
Ryabtseva Alla Alexeevna
Moscow Regional Research Clinical Institute of M F Vladimirsky, Russia
Title: Outcomes of a trifocal intraocular lens implantation in patients with diabetic retinopathy
Time : 14:50-15:02
Biography:
Alla A Ryabtseva is a Doctor of Medical Sciences, Professor, Honoured Doctor of the Russian Federation. An Ophthalmologist, Head of the Ophthalmologic Department of the MONIKI of M F Vladimirsky, Main ophthalmologist of Moscow Region and of the Central Federal District of Russia, a member of editorial councils of the Russian Ophthalmology Journal, Russian Pediatric Ophthalmology and of the Almanac.
Abstract:
Purpose: The purpose is to evaluate the visual outcomes after bilateral implantation of a trifocal intraocular lens in patients with proliferative diabetic retinopathy (PDR).
Setting: All intraocular lens (IOL) implantations were performed at the Ophthalmology Department, Hanoi Russ-Viet Medical Hospital (Mat Viet-Nga), Vietnam.
Methods: This prospective study comprises results after bilateral implantation of the new trifocal aspheric TECNIS Symfony IOL model ZXR00 (Abbott Medical Optics) in 9 patients (18 eyes) with PDR. Diabetes mellitus was in the stage of compensation in all patients. All patients underwent an uneventful cataract surgery followed by IOL implantation by a single surgeon. Postoperative examination including uncorrected distance visual acuity (UDVA), near visual acuity (NVA) and intermediate visual activity (IVA) at 40 cm and 60 cm; defocus testing and spectacle independence was performed.
Results: The mean postoperative binocular UDVA, IVA and NVA at 3 months were 0. 1 log MAR±0.16 (SD), 0.05±0.04 log MAR, and 0.02±0.03 log MAR, respectively. Preoperative spherical equivalent (SE) was +0.22±2.04 D (range: -3.44 to +1.75 D) and postoperative spherical equivalent was -0.19±0.4 (range: -0.75 to 0.13 D). Binocular defocus curve showed best visual acuity (VA) at 0.2 Log MAR or better in the range of +1.5 D to -2.5 D of defocus. 83.3% of patients reported complete spectacle independence and no longer used correction in the far, intermediate, or near distance.
Conclusions: Our study showed that the new-generation trifocal IOL provided high distance, intermediate, and near vision with high rates of spectacle independence in patients with proliferative diabetic retinopathy.
Grishina Elena Evgenievna
M F Vladimirsky Moscow Regional Research Clinical Institute, Russia
Title: Unusual uveal melanoma
Time : 15:02-15:17
Biography:
Grishina Elena is a doctor of Medical Sciences, Professor. Author of more than 200 scientific works. Experience in ophthalmology is 40 years, more than 30 years working as an ophthalmic oncologist, engaged in the diagnosis and treatment of tumors of the eye and its appendage. A member of the European society of ophthalmic oncologists. (European Ophthalmic Oncology Group - OOG).
Abstract:
As a rule, diagnosis of large uveal melanomas does not cause difficulties. Sometimes uveal melanoma mimics other diseases. Then there may be diagnostic errors. The purpose of the work is to report cases of unusual uveal melanomas mimicking other diseases to improve our knowledge about uveal melanomas.
Material: 6 patients aged 37-73 years old had unusual uveal melanomas. In all cases, the diagnosis of uveal melanoma was confirmed morphologically.
Results: An atrophic eye with sluggish uveitis was removed as cosmetics. Uveal melanoma was accidentally detected when histological examination of the enucleated atrophic eye is done. Uveal melanoma simulated traumatic hemorrhagic choroid detachment in 1 patient, 3 patients had unusual growth of uveal melanoma. The growth of a tumor was not in the eye cavity, but it was extrascleral into the orbit One patient was treated with, sluggish uveitis, secondary glaucoma, uveal. There was no effect of the treatment. Due to severe pain syndrome, the blind eye was removed. Diffuse iris melanoma was detected in the enucleated eye.
Conclusion: It is possible to avoid diagnostic errors if to take into account the atypical symptoms of uveal melanoma, its extrascleral growth into the orbit but not into the eye cavity. It is necessary to inspect the enucleated eye intra-op in a microscope. It is important to trace the result of histological examination of the enucleated eye.
Andryukhina Olga Mikhailovna
Moscow Regional Research Clinical Institute of M F Vladimirsky, Russia
Title: Early diagnostics of multiple sclerosis on the basis of changes in choroid
Time : 15:17-15:29
Biography:
Olga M Andryukhina has graduated with Honours from the Medical Faculty of People’s Friendship University of Russia in 2009. Since 2009 till 2011 she studied in the Residency of People’s Friendship University of Russia, the Department of Ophthalmology. Since 2011 Olga Andryukhina has been working in the department of ophthalmology in Moscow Regional Scientific Research Clinical Institute of M.F. Vladimirsky. She is a research associate, published 22 scientific works, and a co-author of three patents and one computer program.
Abstract:
Along with the importance of studies of the retina and optic nerve structure, a special attention is attracted by the state of the choroidal tract of the apple of the eye in patients with multiple sclerosis. As the new possibilities of the choroid visualization have emerged, the interest towards its connection with demyelinating diseases increased. Consequently, the thickness of the choroid became a parameter for the quantitative assessment of the uvea. It can be used to verify the demyelinating processes. It determines the medical and social importance of this research. The present work contains the results of retina and optic nerve examination in 68 patients with relapsing multiple sclerosis and a control group of 23 healthy patients. All the patients underwent an examination of the posterior segment of the eye via optical coherent tomograph (OCT).
Spectralis and a patented method of the quantitative processing of OCT images of the choroid. For the first time the examination of the share of the pore of blood vessels relative to the choroid was carried out in patients with multiple sclerosis, the importance of this factor and the thickness of choroid in the diagnostics of this disease was assessed and a diagnostic model was invented, which increased the index of sensitivity and specificity up to 94.6% and 90.3%. The evaluation of the dynamic pattern of choroid changes received via OCT most brightly characterizes the state of the choroidal tract in this disease and confirms the involvement of the choroidal tract in the pathological process in multiple sclerosis. The changes in choroid thickness and share of the pore of blood vessels relative to the choroid can predict the neurodegenerative processes in the retina and optic nerve. As a result, using of integrated approach to the multiple sclerosis diagnostics, it is important not only to analyze the parameters of the optic nerve, but also the state of the choroid.
Sidorenko Evgeniy Evgenich
Pirogov Russian National Research Medical University, Moscow, Russia
Title: Treatment of retinopathy of prematurity with aflibercept in Russia
Time : 15:29-15:41
Biography:
Sidorenko Evgeny Ivanovich - corresponding Member of the Russian Academy of Sciences, Honored Scientist of Russia, Honored Doctor of Russia, Professor, Med.Sc.D., Head of the Department of Ophthalmology of the Pediatric Faculty Russian National Research Medical University by name N.I. Pirogov, Member of the European Society of ophthalmologists, Coordinator of the intergovernmental German-Russian Commission on medicine and the international Alliance of highly developed countries in medicine M8, Founder and editor-in-chief of the Journal "Russian Children Ophthalmology". Author of 668 articles, 27 monographs and 7 textbooks, 56 patents. He has supervised 16 theses Med.Sc.D. and 52 PhD. Scientific activities: perinatal ophthalmology, retinopathy of prematurity, pathology of the visual and nervous apparatus of the eye, hypoxic conditions in ophthalmology, neuroophthalmology, refractive surgery, laser surgery, laser treatments for diseases of the optic nerve and congenital glaucoma. He was awarded the medals of Ehrlich and Albert Koch (2006) for the discovery of infrasonic phonophoresis phenomena.
Abstract:
Introduction: In 2016 for the first time in Russia, we began to use aflibercept (VEGF) for the treatment of retinopathy of prematurity. Despite the current scientific and technological progress achieved in neonatology and intensive care, a premature baby often suffers from severe comorbidities that generally lead to early disability already in childhood. One of the most common causes of childhood blindness and vision impairment is retinopathy of prematurity (ROP). In developing countries with middle-income, such as Latin America, Eastern Europe, India and China, ROP is considered to be the leading cause of child blindness. In most countries laser photocoagulation has largely replaced the cryotherapy of the peripheral avascular retina and is recognized as the standard of treatment for ROP. Recently vascular endothelial growth factor (VEGF) has been recognized as the key factor in the pathogenesis of ROP. Inhibitors of VEGF (anti- VEGF drugs) are widely used in ophthalmology for treatment of retinal diseases associated with neovascularization and macular edema. Aflibercept use for ROP treatment potentially may have several advantages. Aflibercept molecule was specially designed for strong, broad and long-lasting anti-angiogenic activity.
Material and Methods: This study is retrospective observational consecutive case series. The study included 132 (264 eyes) infantswith retinopathy of prematurity (ROP) who were hospitalized and received treatment at «Scientific and Practical Center of Pediatric Specialized Medical Care» in Moscow between October 2016 and November 2017. All patients were treated with single dose of intravitreal aflibercept 0.6 mg/0.015 ml. Additional injections were possible if recurrence of retinopathy of prematurity occurred defined as following: recurrence of vascular activity in central and peripheral zones of the retina. Exudation and proliferation in central zone of the retina and on the border with avascular zones. This includes formation of arteriovenous fistula and fibrous tissues (epiretinal membranes). Intravitreal aflibercept injections were performed in operating room settings. Specialized equipment was used for anesthesia of infants with low and extremely low weight. Three days prior aflibercept injection all infants received topical antibiotics (Levofloxacin, 0.5%) and atiseptic (Picloxydinum, 0.5 mg) 1-2 drops 4 times a day applied epibulbar in both eyes. Intravitreal injection was performed according to the standard technique. Prior the injection skin was prepared with antiseptic solution (Octenisept) followed by the epibulbar antibiotic application. Blepharostat was used. After the injection tamponade of injection site was performed. Antibiotic ointment (Ofloxacin, 0.3%) was applied to lower eyelid. After the aflibercept injection and during 7 days following the injection all infants received antibiotics (Levofloxacin, 0.5%) and antiseptic (Picloxydinum, 0.5 mg) 1-2 drops 4 times a day applied epibulbar in both eyes.
Results: 132 patients (264 eyes) with retinopathy of premature were treated with intravitreal aflibercept 0.6 mg/0.015 ml used as monotherapy. 51 infants (38.64%) were female. Mean gestational age at birth was 27.62 ±2.44 weeks. Mean postconceptual age at the moment of first aflibercept injection was 40.11±5.88 weeks. Most of the patients (71.97%) had stage 3+ retinopathy. Baseline demographic and clinical characteristics are summarized in table 1. Out 132 patients only 106 patients (212 eyes) have completed observation period and reached 55 weeks of postconceptional age. Therefore 26 patients were not evaluated for complete vascularization of 3 retina zones at the postconceptual age of 55 weeks. Four patients did not reach 55 weeks of postconceptional age and were withdrawn from observation due to the fatal outcomes. 22 patients did not reach 55 weeks of postconceptional age due later treatment initiation and therefore shorter observation period.
Conclusion: Intravitreal aflibercept 0.6 mg potentially is an effective treatment for retinopathy of prematurity that potentially will prevent child blindness. Use of anti-VEGF for ROP treatment has several advantages in contrast to laser photocoagulation that include ability to reduce the anesthesia time to 5 minutes, absence of retinal damage, absence of need for expensive equipment, the lack of long training on expensive equipment.
Nazarenko Anastasia Olegovna
Pirogov Russian National Research Medical University, Moscow, Russia
Title: Resistance of the organ of vision to bevacizumab (Avastin) in its systemic use in children with solid malignant tumors
Time : 15:41-15:53
Biography:
Nazarenko Anastasia Olegovna MD is a Resident of the Department of Ophthalmology of Pirogov Russian National Research Medical University. She graduated from Peoples’ Friendship University of Russia in 2017. Her scientific interests includes: retinopathy of prematurity, myopia and prophylaxis of the diseases.
Abstract:
Since 2009, the Oncology Department of Scientific-Practical Center of Specialized Medical Care for Children named after V F Voino-Yasenetsky, within Pirogov Russian National Medical Research University is treating malignant tumors in children using bevacizumab (Avastin) according to the approved protocols. In 2011, for the first time in Russia, after evaluating the effect of bevacizumab (Avastin) on the resistance of the eye tissues in children with cancer we decided to use bevacizumab (Avastin) for the treatment of retinopathy of prematurity. By this time, there were only a few publications on this topic in the world and none in Russia. For the treatment of the children with cancer, bevacizumab (Avastin) was used systemically in the large doses of (5-15 mg/kg). The research includes the examination of 25 patients aged 3 to 17 years with malignant solid tumors of the brain, lungs, bones and nasopharynx. It was discovered that the systemic use of high doses of Avastin does not affect the tissues of the eye and its function but rather it showed a greater resistance to angiogenesis blockers. Changes in the eyes only reflected the dynamics of the tumor process. These studies allowed us to proceed to the intravitreal administration of Avastin for patients with the retinopathy of prematurity.
Rosello Quesada Nicholas Manuel
Pirogov Russian National Research Medical University, Moscow, Russia
Title: Botox therapy in case of strabismus in children
Time : 15:53-16:05
Biography:
Nikolas Manuel Roselo Kesada is a Postgraduate of the Department of Ophthalmology of Pirogov Russian National Research Medical University (RNRMU). He was graduated from Pirogov Russian National Research Medical University of Russia in 2017. He is working on PhD thesis entitled as: Further results of oculomotor disorders treatment with botulotoxin injections in children.
Abstract:
Introduction: Strabismus causes a cosmetic defect, a violation of binocular vision, forms amblyopia. To date, there is no sufficiently effective therapeutic method for treating strabismus. Traditional surgical treatment is traumatic, and it is not always possible to achieve the desired result. The aim of the study was to study the effectiveness of Botox injections with a friendly strabismus in children. The inclusion criteria were an alternating strabismus. An exclusion criterion includes paralytic, non-accommodative strabismus and nystagmus.
Material & Methods: All patients with strabismus were under the supervision of ophthalmologists, pediatricians. This type of treatment was approved by the ethical committee of the Pirogov Russian National Research Medical University and the Scientific Council of the Voino-Yasenetski Scientific and Practical Center for Children's Specialized Medical Care. The written informed consent of the parents was also received. 121 operations were performed in 104 children between 2016 and 2018. 56 patients were girls (53.85%). 48 patients were boys (45.15%). The average age was 3.2 years. Divergent strabismus was diagnosed in 15 patients (14.42%). Convergent strabismus was diagnosed in 89 patients (85.58%). Three groups of patients: Group 1: 9 patients (8.65%) with a deviation angle of up to 15; Group 2: 30 patients (28.85%) with deviations with an angle of 15 to 25; Group 3: 65 patients (62.5%) with deviations with an angle of 25 or more; The average deviation angle in group 1 was 12.7; in 2nd groups - 22 and in 3rd group - 37.7 degrees. The examination was carried out before the injection, at 1, 2 and 3 days after the procedure. Further observations were carried out once every two weeks. Botulinum toxin injection was given to children in accordance with standard methods. The skin was treated with an antiseptic solution (octenisept), epibulbar applied antibiotics. Electromyography was used during the injection to make sure that the injection was made into an isolated muscle under mask anesthesia (Sevoflurane). After the injection of botulinum toxin and for 7 days all patients have access to antibiotics (Levofloxacin, 0.5%) and antiseptic (Picloxydine, 0.5 mg) 1-2 drops 4 times a day epibulbar in both eyes. The first injection of botulinum was carried out at a dose of 2.0 units for direct muscles and depending on the individual effect, for repeated application of 2.0 to 6.0 units in each muscle.
Results: Repeated injections of botulinum toxin were performed in 20 patients (20.8%). Complications were noted: scleral hemorrhage in 41 patients (39.4%); short-term ptosis in 74 patients (71.15%); contralateral alternating strabismus was noted in 98 patients (94.23%). Ðll complications are reversible and predictable in the postoperative period. Horizontal strabismus (esophoria, exophoria) became less pronounced in 96 patients (92.31%), complete regression with restoration of binocular functions was noted in 54 patients (51.92%).
Conclusions: This method allows you to correct strabismus in children in a short period of time, with minor trauma and effectively create conditions for the formation of physiological binocular vision.
Levchenko Yuliya Sergeevna
Krasnoyarsk Clinical Ophthalmological Hospital, Krasnoyarsk, Russia
Title: Evaluation of the disinfecting properties of solutions for the care of soft contact lenses
Time : 16:05-16:15
Biography:
Yuliya S. Levchenko, has completed his PhD at the age of 28 years from Krasnoyarsk Medical University. She is an ophthalmologist doctor at Krasnoyarsk clinical ophthalmological hospital named after P.G. Makarov. Selects all kinds of contact lenses, including toric, multifocal and orthokeratological lenses. Author of 20 scientific works on contact correction of vision. Currently he studies safety for the eyes when using contact lenses and solutions for them.
Abstract:
Contact vision correction is an effective method of correction of refractive error, therefore more than 130 million people in the world use contact lenses. However, there is a complication problem in contact correction (toxic-allergic, infectious), which is caused by insufficient daily cleaning of surface deposits on lenses and their disinfection with the help of disinfectants used for lens washing. Bioluminescent analysis, which is based on quenching the bioluminescent glow of the bacterial enzymatic test system in response to the addition of the solution under analysis, can be used to identify the disinfecting properties of the solutions used for contact lenses care. The purpose of the study is to identify the possibility of using bioluminescence analysis of determining the disinfectant properties of universal solutions used for contact lenses care. Universal solutions for washing contact lenses of Russian and foreign production, including Spain, Great Britain, were studied. The solutions were tested both before use (just after opening the vial) and after use by soaking contact lenses (produced in the UK), which were in use for 14 days, 1 month and 3 months. The bacterial bio enzymatic system NADH:FMN-oxidoreductase + luciferase (Krasnoyarsk, Russia) was used as a test system. The biotest reaction was determined by the amount of inhibiting the bioluminescent test system. It is established that just after opening the vial; the universal solutions for washing contact lenses of Russian production inhibited the bioluminescence glow less than the solutions of foreign production. A high percentage of inhibition of bioluminescence glow indicated the destruction of protein enzymes that were in the test system, which in its turn indicated good disinfecting properties of the solutions. The analysis of the solutions after soaking contact lenses revealed that bioluminescent glow was intensified from the solutions of Russian production, so the contact lenses immersed in them were not cleaned enough. Bioluminescent glow of the solutions of foreign production did not change, i.e. their disinfecting properties preserved. In addition, there is an increase in inhibiting bioluminescence glow with growing wear time. We explain it by accumulation of deposits on contact lenses. Thus, the enzymatic test system applied for testing luminous bacteria can be used as a diagnostic integral indicator of disinfecting properties of universal solutions for contact lenses care and can be a promising direction in clinical ophthalmology for studying the causes of complications in contact correction of vision.
Recent Publications
1. Global Industry Analysts, Сontact lenses and solutions: A Global Strategic Business Report, June 2014.
2. Alipour F, Khaheshi S, Soleimanzadeh M, et al. (2017) Contact lens-related complications: a review. Journal of Ophthalmic and Vision Research 12(2):193–204.
3. Narayana B L, Rao P, Bhat S, et al. (2018) Comparison of the antimicrobial efficacy of various contact lens solutions to inhibit the growth of Pseudomonas aeruginosa and Staphylococcus aureus. International Journal of Microbiology DOI: 10.1155/2018/5916712.
4. Kratasyuk V and Esimbekova E (2015) Applications of luminous bacteria enzymes in toxicology. Combinatorial Chemistry & High Throughput Screening 18(10):952-959.
Ali-Zadeh Giunel Khaganovna
Moscow Regional Research Clinical Institute of M F Vladimirsky, Russia
Title: Cytological control of the effectiveness of the treatment of dry eye disease
Time : 16:15-16:27
Biography:
Ali-zadeh Giunel Khaganovna has completed Azerbaijan Medical University, then graduated from internship at City Clinical Hospital, Azerbaijan. Currently working as an Ophthalmologist at Moscow Regional Research Clinical Institute of M F Vladimirsky, Russia
Abstract:
Traditionally, in medical practice, much attention is paid to morphological methods of diagnosis. Differential morphological diagnosis takes into account the signs of the norm, borderline states and the actual pathological signs, depending on the degree of their severity. One of the classical morphological methods is a cytological study. The main characteristics of the cytological method of investigation make it possible to use it in ophthalmology, namely in the diagnosis and monitoring of diseases of the anterior surface of the eye. One of the actual problems is dry eye syndrome (DED). The study involved 60 patients, 55 of them women, 5 men aged 25 to 80 years with a clinical diagnosis: Dry eye syndrome. The control group was 12 people. At the beginning of the study, all patients underwent a comprehensive ophthalmological examination, which included the collection of an anamnesis for ophthalmic and general diseases. All patients were monitored for one to four months and the following types of examinations took place: assessment of subjective improvement in the ocular surface disease index (OSDI) questionnaire, fluorescein and lissamine green stains, determination of the rupture time tear film (VRSP) and the Schirmer test to determine the positive dynamics of objective indicators. The above studies were carried out during each visit. In this study, first of all, the use of Aktipol for the treatment of the inflammatory component of the dry eye syndrome was evaluated. In a clinical trial, it was found that the administration of Actipol for topical administration significantly reduced the subjective and objective manifestations of dry eye syndrome in patients with a deficiency of the aqueous component of the tear and dry keratoconjunctivitis. These observations were confirmed by the cytological method of investigation.
